Surprising fact: up to half of these targeted injections can fail on at least one side, yet many patients still gain meaningful relief.
The pudendal nerve block is an outpatient injection in the pelvic region that aims to interrupt pain signals and provide focused regional anesthesia for select gynecologic, obstetric, and anorectal procedures.
Results vary by person: some patients get significant pain relief that lasts weeks to months, while others notice only brief benefit. The method is commonly used for chronic pelvic pain and targeted anesthesia during childbirth and repair of tears.
Providers review risks and typical side effects, which are usually mild. Serious complications are rare when experienced clinicians perform the procedure.
For a detailed clinical review and background, see the clinical review. For practical patient-focused notes on injecting for pain control, read what to know about nerve root.
Key Takeaways
- The procedure is a targeted outpatient injection to numb the pelvic area for pain relief.
- Outcomes differ—some patients have lasting benefit, others only short-term relief.
- Common uses include chronic pelvic pain and anesthesia during childbirth-related care.
- Typical side effects are uncommon and usually mild; major complications are rare.
- Discuss candidacy and alternatives with your clinician to make an informed choice.
Overview: Targeted pain relief for the pelvic region
Clinicians use a precise injectable technique to limit pain where it matters most during certain pelvic procedures.
What it does: This targeted regional anesthesia numbs tissues of the perineum, lower vagina, and rectum to provide focused pain relief during and after select procedures.
Compared with broader options like epidurals, this approach gives localized coverage. That often means less whole-body medication and a quicker recovery for the patient.
Common uses include late labor care, episiotomy repair, instrument-assisted delivery, and select anorectal procedures. Effectiveness varies by anatomy, condition treated, and technique, so not every person experiences the same duration or degree of relief.
Outpatient experience: A short pre-procedure check, a quick injection with brief monitoring, and same-day discharge are typical. When done by trained clinicians using sterile technique and imaging, safety and accuracy improve.
This option is one part of a larger pain plan. Patients should discuss goals, expectations, and alternatives with their care team before scheduling.
What is a pudendal nerve block?
A targeted injection helps test and treat pelvic pain by numbing a small, defined area.
Definition and purpose in regional anesthesia
This procedure places local anesthetic near the pudendal nerve to temporarily interrupt pain signals from the perineum, genitals, and rectum.
Purpose: It provides highly localized regional anesthesia for specific childbirth and minor anorectal procedures. Clinicians also use it diagnostically to see if the affected area is the source of chronic pelvic pain or neuralgia.
How it differs from an epidural or spinal
Unlike epidural or spinal techniques that act at the spine, this approach numbs only a focused area. Mobility is usually preserved, and leg strength is less affected.
- Quick onset of numbness in the intended distribution.
- Duration depends on the anesthetic chosen.
- It does not relieve uterine contraction pain and is not a replacement for epidural analgesia during active labor.
| Feature | Target | Mobility | Typical uses |
|---|---|---|---|
| Focused injection | Perineum, genitals, rectum | Preserved | Episiotomy, minor anorectal procedures, diagnostic pain testing |
| Epidural/spinal | Spinal nerve roots | May reduce leg strength | Labor analgesia, major pelvic surgery |
| Practical outcome | Short, site-specific relief | Can walk | Part of multimodal care |
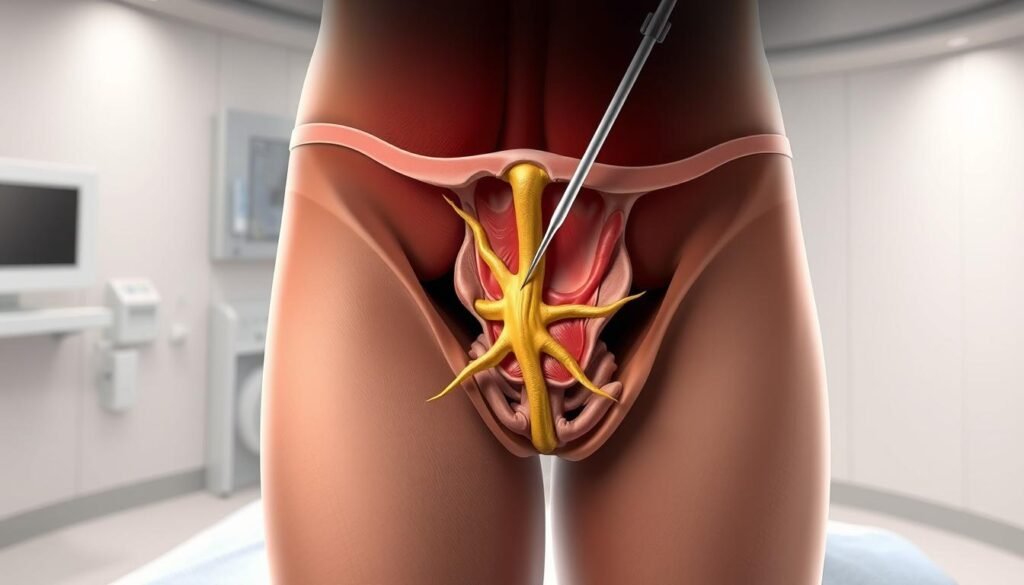
Pudendal nerve anatomy and why it matters
A winding course through ligaments and bony landmarks makes accurate placement essential for effective pain relief.
The pudendal nerve arises from the sacral plexus, leaves and then re-enters the pelvis, and follows a complex pathway into the perineum. This route explains why precise landmarking matters when targeting a small area for anesthesia.
Key branches and their roles:
- Inferior rectal nerve — supplies the anal sphincter and nearby skin, often linked to rectal pain.
- Perineal nerve — serves the perineum and external genitalia and contributes to sensation and motor function.
- Dorsal nerve of the clitoris/penis — carries sensation for the clitoral or penile region.
Clinicians commonly aim near the ischial spine beside the sacrospinous ligament because the pathway is more accessible there. Side-to-side anatomic differences are common and can change where a person feels pain and where a block will be most effective.
Palpation and imaging help confirm the position relative to bony landmarks before medication is delivered. Knowing the sensory map predicts which procedures or symptoms in the region will get the best relief.
When a pudendal nerve block is used
This targeted injection has clear roles in obstetric care, chronic pelvic conditions, and diagnostic testing.
Childbirth applications: In the second stage of labor, providers may use the procedure to reduce perineal pain during pushing, episiotomy repair, or assisted deliveries. It does not relieve contraction pain and may also be used when broader anesthesia is unnecessary.
Chronic pelvic pain indications: People with pudendal neuralgia, vulvodynia, or proctalgia fugax may try this technique when localized symptoms persist. A successful injection can interrupt pain signals long enough to begin physical therapy or adjust medications.
Diagnostic value: Meaningful short-term relief after the injection often suggests the pudendal nerve is a pain source. That information helps clinicians tailor ongoing care and consider options for nerve entrapment or other causes.
Considerations in men: Men may report penile, scrotal, perineal, or rectal pain linked to trauma or cycling microtrauma. In those cases, targeted injections can both confirm the diagnosis and provide therapeutic relief while other treatments are planned.
- Obstetric use: focused perineal anesthesia during the second stage.
- Gynecologic/anorectal: short-term numbness for select repairs.
- Chronic pelvic pain: pudendal neuralgia, vulvodynia, proctalgia fugax.
- Diagnostic: relief after injection supports targeted care.
Who is a good candidate
Candidacy starts with a focused evaluation that links symptoms to a clear sensory map of the perineal area.
Evaluation, medical history, and imaging guidance
Ideal candidates have localized pain or procedural needs inside the pudendal nerve distribution and want a targeted treatment that may reduce systemic medication use.
- Pre-procedure review: medical history, current medications (especially blood thinners), allergies, and prior response to injections.
- Physical exam: symptom mapping confirms the area of greatest pain matches the expected distribution.
- Imaging guidance: ultrasound often improves accuracy and safety, especially in altered anatomy or challenging body habitus.
Clinicians discuss realistic goals and timelines so the patient understands how much relief is likely and how the procedure fits into broader pain management plans.
| Quick check | Yes = proceed | No = caution |
|---|---|---|
| Symptoms map to distribution | Yes | No |
| Safe medical profile | Yes | Active infection or bleeding risk |
| Imaging feasible | Ultrasound available | Poor visualization |
Contraindications include infection at the site and uncontrolled coagulopathy. Follow-up planning evaluates benefit and next steps in cases where relief is partial or temporary.
The procedure: techniques and guidance
Clinicians choose a specific technique based on anatomy, patient needs, and the target site near the ischial spine. A short consult explains the approach and expected effects on pain in the perineal region.
Transvaginal versus transperineal approaches
Transvaginal access is common in obstetric and gynecologic settings. It offers a direct path for many patients.
Transperineal entry is used for men and when external access is preferred. Both routes aim the medication near the ischial spine and sacrospinous ligament.
Image guidance: ultrasound or fluoroscopy
Imaging helps confirm placement and lowers risk. Ultrasound is commonly used for real-time visualization and avoids radiation. Fluoroscopy may be chosen when bony landmarks need clearer reference.
Medications and technique steps
- Typical medicines: lidocaine or bupivacaine as a local anesthetic; some clinicians add dexamethasone or triamcinolone to extend effect.
- Stepwise process: positioning, skin prep, local skin anesthetic, careful advancement of the needle, test aspiration, slow injection of anesthetic and any steroid.
- Safety checks include patient feedback during advancement and brief monitoring after the procedure.
For detailed technical notes, see this clinical technique review.
What to expect before, during, and after the injection
A clear pre-procedure routine helps reduce anxiety and sets expectations for sensations during the injection.
Sensations during the procedure
Before the injection, the clinician will position you and cleanse the skin with a sterile solution such as chlorhexidine.
Expect a brief stinging from the local skin anesthetic. That sting fades quickly.
“You may feel a short pressure sensation as medicine spreads, then numbness and tingling before pain eases.”
After the pressure, numbness follows in the targeted area. Some patients notice warmth or mild tingling as the goal of short-term relief begins.
Recovery timeline and post-care
Effects usually last several hours, often between 4 and 24 hours, depending on the medicine used and individual response.
- Monitor for mild soreness or bruising at the injection site; this often fades within a day.
- Avoid heavy lifting, strenuous exercise, and sexual activity for about 24 hours.
- Make sure you have a safe ride home if sedation or dizziness occurs.
After a short observation period, the patient is typically discharged the same day. Call your provider if you develop fever, increasing pain, spreading redness, or other signs of infection.
Note: Some patients get longer relief when steroids are added; others find benefit is short-lived. Discuss expectations and follow-up plans before you leave.
Benefits, risks, and side effects
Knowing the balance of expected benefit and possible harm helps patients make an informed choice.
Potential benefits
Targeted pain relief during childbirth-related procedures or minor anorectal care often reduces the need for oral or IV medicines.
This focused option can shorten recovery and limit systemic side effects from opioids or large-dose analgesics.
- Diagnostic value: short-term improvement helps confirm a nerve contribution such as neuralgia.
- Outpatient recovery with minimal downtime in most cases.

Possible risks and how clinicians reduce them
Risks are uncommon but include localized infection, bleeding or hematoma, allergic reactions to the anesthetic, and rare nerve injury.
“Serious complications are rare when clinicians use sterile technique and imaging guidance.”
- Risk reduction: sterile prep, careful aspiration, and imaging lower unintended effects.
- What you may also notice: mild soreness or bruising that usually resolves quickly.
- In select cases, relief can outlast numbness — possibly due to reduced local inflammation and muscle guarding.
Return precautions: escalating pain, fever, spreading redness, or new neurologic changes warrant prompt contact with your care team.
How long does relief last and can blocks be repeated?
Relief after a targeted injection often starts quickly, but the exact time frame varies by person.
Most people feel numbness and reduced pain for several hours—commonly between 4 and 24 hours. When clinicians add a steroid, some patients report benefit that lasts days to weeks.
Why duration varies: the chosen medicine and dose, individual anatomy, and whether neuralgia is active all change results. In chronic pelvic conditions, a single procedure can give a useful break in the pain cycle and allow other treatments to begin.
Repeat strategy: nerve blocks may be repeated when benefit is clear. Clinicians space repeat injections based on response, overall treatment goals, and cumulative steroid exposure. They will also weigh bleeding risk and other safety side considerations.
- Typical duration: hours; with steroid, days to weeks.
- Role in chronic pelvic care: a window to start pelvic floor therapy or posture and activity changes.
- If relief is brief: discuss alternative nerve blocks, different medicines, or advanced options with your provider.
Conclusion
A well-placed, image-guided injection can reduce pain in the perineum and help confirm the source of symptoms.
In short, a pudendal nerve block is a minimally invasive option that delivers a local anesthetic near the ischial spine to give targeted pain relief for certain perineal procedures and chronic pelvic pain.
The procedure uses sterile skin prep, ultrasound or fluoroscopy guidance, and careful needle placement. Patients may feel a brief pressure sensation, followed by temporary numbness in the treated area.
Most side effects are mild and brief. When pain improves, the injection can guide further treatment such as physical therapy or medication adjustments. Discuss risks, expected duration, and repeat options with your care team to decide if this focused procedure fits your pain management plan.

