If persistent pain has reshaped your days, you are not alone. Many people reach a point where physical therapy, meds, and injections no longer bring real relief. That moment can feel discouraging and also open the door to thoughtful next steps.
This advanced neuromodulation option is meant for people whose chronic pain has not improved with conservative care. It is not a first-line choice, but a considered path when other approaches fall short.
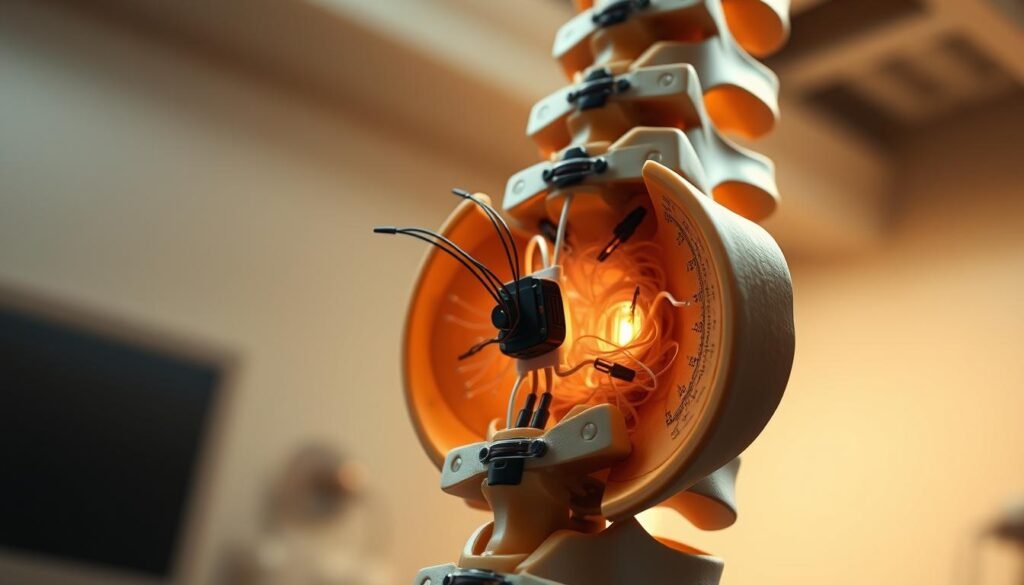
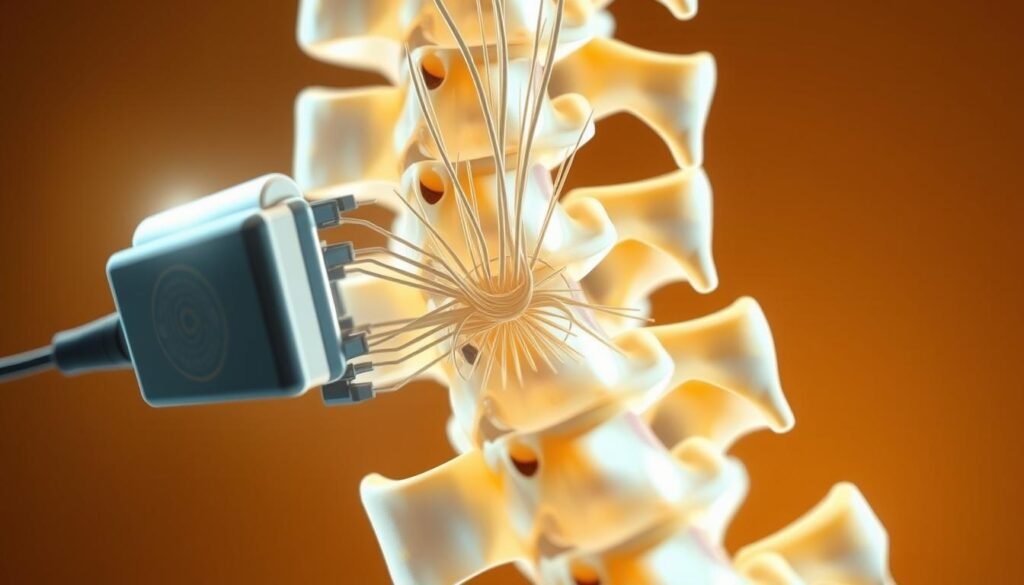
The system uses thin leads placed in the epidural space to influence how pain pathways behave. Those leads connect to a small implanted generator under the skin that clinicians program and adjust during follow-up.
Care usually follows a two-step path: a short trial to test benefit, then a minimally invasive implant if the trial gives at least 50% improvement. Most people go home the same day after the trial and within a day or two after the surgery.
Goals focus on making pain more manageable and improving quality of life, not curing the underlying condition. A multidisciplinary team helps with candidacy, the procedure, and ongoing programming, and some systems need periodic charging or eventual battery replacement.
Keep reading to learn who qualifies, how to prepare, what to expect during the trial and implant, and how recovery and long-term care are supported.
Key Takeaways
- This option is for persistent pain that hasn’t responded to conservative care.
- A short trial comes first; a permanent implant follows if the trial helps.
- Leads in the epidural space link to a small, programmable generator under the skin.
- Most patients go home the same day after the trial and soon after implant surgery.
- The aim is better pain management and life quality, supported by a care team.
What a Spinal Column Stimulator Is and How It Helps Chronic Pain
A small, implanted system can change how your body sends painful messages to the brain. The device delivers low-level electrical pulses near the spinal cord so fewer pain signals reach the brain. This neuromodulation can reduce the intensity of chronic pain and help you do more daily activities.
Neuromodulation basics: interrupting pain signals to the brain
Think of the pulses as a volume knob for pain. Gentle current alters nerve activity so the brain receives fewer or weaker pain messages. Many people notice less discomfort without taking stronger medicines.
Key components: leads, pulse generator, and programming
Leads are thin wires with contacts placed in the epidural space near the cord. A small pulse generator sits under the skin and links to the leads with tunneled extensions.
“Programming is the smart part — clinicians tune settings to target specific painful areas and activities.”
- Placement depends on pain location: thoracic for lower back and legs, cervical for arm or neck symptoms.
- Modern programs often feel minimal; any mild tingling usually fades over time.
- Battery options: rechargeable units may last 10–15 years; non-rechargeable types often need replacement at 3–5 years.
| Component | Function | Typical Lifespan |
|---|---|---|
| Leads | Deliver pulses to nerve tissue near the cord | Remain unless moved or replaced |
| Pulse generator | Produces and controls stimulation | 3–15 years (depends on type) |
| Programming | Customizes patterns for pain coverage | Ongoing, adjusted at follow-ups |
Who Is a Candidate for Spinal Cord Stimulation
When standard therapies fail, clinicians look for specific patterns that predict benefit from cord stimulation.
Common candidates include people with persistent back pain or neck pain, failed back surgery syndrome, complex regional pain syndrome (CRPS), and neuropathic or nerve pain such as painful diabetic neuropathy.
Referral often starts after about six months of disabling symptoms that do not improve with medications, physical therapy, or injections. Primary care providers typically refer patients to a pain specialist for evaluation.
https://www.youtube.com/watch?v=Vluvyif1mBg
Who may not be a good fit
If imaging shows a correctable structural problem and surgery would likely help, corrective surgery is usually preferred before considering cord stimulation. Uncontrolled psychiatric illness or active infection can also reduce success.
How neuropathic pain looks
Neuropathic patterns—burning, shooting, throbbing, or marked sensitivity to light touch—often respond well to spinal cord stimulation when injured nerves keep sending pain despite healing.
“The goal is to match the right treatment to the right condition, offering this device only after other options have been tried or ruled out.”
- A multidisciplinary team confirms other treatments were attempted and that no better surgical option exists.
- Systemic causes, like diabetes-related nerve injury, are reviewed before recommending a trial of cord stimulation.
Pre‑Procedure Evaluation and Care Team
Before any implant, a coordinated team evaluates your medical risks and readiness for the procedure. This step keeps you safe and helps the team plan the best approach.
Who you may meet:
- Neurology to confirm the pain diagnosis and prior treatments.
- Pain management to review options and coordinate the trial.
- A neurosurgeon to discuss the implant and perform the surgery.
- A psychologist or psychiatrist to assess mental health factors that affect outcomes.
- An anesthesiologist to tailor anesthesia and review your medical history.
Key tests prepare the team and reduce risk: labs, imaging (x‑ray or MRI as needed), and an EKG to check cardiac rhythms. These checks help the surgeon and anesthesiologist plan safely.
Prep, medications, and infection prevention
Make sure you list all medications and supplements. Your clinician may ask you to pause blood thinners only under medical guidance.
Fasting is usual: no solid food for eight hours and no liquids for two hours before anesthesia. Use any pre‑op skin‑cleansing products as directed to lower infection risk.
“A psychological assessment can improve satisfaction with cord stimulation by identifying and treating mood or sleep issues beforehand.”
Bring questions to each visit so you understand the timeline and home responsibilities. Clear communication with the team supports safe care and a smoother procedure.
Spinal Column Stimulator: The Trial Procedure
A short outpatient trial gives practical feedback on whether electrical stimulation meaningfully lowers your symptoms.
How the trial starts:
Fluoroscopic guidance and percutaneous lead placement
Most trials are done the same day and use fluoroscopy so the clinician can place temporary leads through a small skin opening. You usually have light sedation and local anesthesia. A specialized needle guides the lead into the epidural space along the spine.
External connection and testing
The temporary lead exits the skin and links to a small external generator attached with glue or sutures. Programming begins right away so different settings are tested over several days.
Timing and defining success
Trials typically last about a week. You’ll keep a pain diary and track activity each day. A trial is considered successful when pain drops by at least 50%. If this trial is successful, the team usually schedules permanent implantation within a week or two.
Paddle electrodes and overnight stays
If percutaneous placement is not possible, a surgeon may place a paddle electrode. That approach is surgical, needs a small incision, and often requires an overnight stay for monitoring and comfort.
“Most people report only mild soreness at the insertion site; staff provide clear home-care steps to keep the dressing dry and reduce infection risk.”
Home-care tips:
- Keep the dressing dry and avoid heavy lifting or twisting that might move the lead.
- Secure the external device as instructed and check the site daily for redness or drainage.
- Call your clinician for fever, increasing pain, or signs of infection.
| Step | What to expect | Typical timing |
|---|---|---|
| Placement | Fluoroscopic percutaneous lead with light sedation | Same day, outpatient |
| Testing | External generator programmed and adjusted | Several days to one week |
| Decision | 50% or more pain relief -> schedule permanent implant | Within 1–2 weeks if successful |
| Paddle option | Surgical electrode with small incision and overnight stay | Hospital observation: 1 day |
For more on how effective a trial can be, read a short review of trial outcomes at trial effectiveness.
Implantation Surgery: From Leads to Pulse Generator
The permanent implant is a planned, one‑day procedure that follows a successful trial and aims to lock in the coverage that reduced your symptoms.
General anesthesia and incision locations
Most patients have the procedure under general anesthesia so the surgeon can work precisely. The team makes a small midline incision in the back where the trial leads gave the best coverage.
A second incision is made near the waist or upper buttock to create a pocket for the pulse generator. The placement is chosen for comfort and easy access for charging or remote use.
Lead anchoring, tunneling under the skin, and generator placement
The surgeon re‑creates the trial lead position and secures the leads with anchors to reduce migration. Connectors are tunneled beneath the skin to the generator pocket for a neat, low‑profile finish.
Secure fixation and tunneling protect wires beneath skin and help minimize irritation. Imaging guidance helps optimize lead position to cover the painful area while limiting tissue disruption.
Rechargeable vs. non‑rechargeable batteries and device control
Generator options include rechargeable units, which can last over a decade with routine at‑home charging, and non‑rechargeable types that often need replacement every 3–5 years.
Most devices offer remote control for on/off and program changes. Initial programming may occur in the OR or recovery room, with fine tuning at follow‑up visits to match your daily routines and pain map.
“Your surgeon will pick the generator site with your hand dominance, sleep posture, and comfort reaching the device in mind.”
| Step | What happens | Why it matters |
|---|---|---|
| Incisions | One over the midline back and one near the waist/buttock | Allows lead placement and a reachable generator pocket |
| Anchoring & tunneling | Leads are fixed and connectors tunneled under skin | Reduces lead movement and protects wires |
| Generator type | Rechargeable or non‑rechargeable battery | Trade‑off: longevity vs. future replacement |
| Programming | Initial in OR/recovery, refined at follow‑ups | Optimizes coverage for daily activities |
Aftercare note: Expect mild soreness for a few days. Your team will give medication guidance, wound‑care instructions, and movement limits to support healing.
To learn more about conditions that may benefit from this procedure, see conditions that qualify.
Recovery, Activity, and Follow‑Up Care
The days after your procedure are about protection, pacing, and learning how the device fits into daily life.
Hospital stay and timelines: After a successful trial most people go home the same day or the next day. Following permanent implantation, discharge usually happens within one or two days.
Wound care matters. Keep incisions clean and dry and change dressings as instructed for 7–10 days.
Return for a clinic visit around 10–14 days so the surgeon can remove staples or sutures and check healing.
Activity limits and safe movements
Limit bending, lifting, and twisting for about 4–6 weeks to reduce the risk of lead movement. Gradually resume normal activities with your care team’s guidance.
Use log‑rolling to get in and out of bed, avoid overhead reaching early on, and support the generator area when coughing or sneezing.
Programming adjustments and device education
Before discharge you will learn how to use the remote, charge a rechargeable generator, and switch programs.
Early follow-up visits focus on programming adjustments to optimize pain relief during daily activities, work, and sleep.
“Mild soreness is common and usually improves in days; regular follow‑up helps fine‑tune settings for better comfort.”
When to call your doctor: Report fever, growing redness, drainage, severe or new pain, new weakness, or balance changes right away to catch problems early.
| Topic | What to expect | Timing | Why it matters |
|---|---|---|---|
| Hospital stay | Same day after trial; 1–2 days after implant | Day 0–2 | Ensures early recovery and monitoring |
| Wound care | Keep dry, change dressings 7–10 days | 1–2 weeks | Reduces infection risk and promotes healing |
| Activity limits | No bending/lifting/twisting | 4–6 weeks | Prevents lead movement and device issues |
| Follow‑up | Programming and incision check | 10–14 days and periodic visits | Optimizes pain relief and long‑term comfort |
Risks, Complications, and When to Call Your Doctor
Understanding possible complications helps you spot problems early and act quickly. Below are common issues, ways to reduce them, and clear red flags to report right away.
Common risks to watch for
- Infection or bleeding at incision or skin sites.
- Cerebrospinal fluid (CSF) leak causing positional headache.
- Lead migration, breakage, or generator problems that reduce benefit.
- New or persistent tingling, numbness, or altered sensation near nerves.
Prevention and simple steps
Follow pre‑op skin prep, take antibiotics if prescribed, and keep dressings clean and dry. These steps lower infection risk and protect healing.
Red flags — call your team immediately
- Fever above 100.0°F or chills.
- Severe headache that worsens when standing or improves when lying down (possible CSF leak).
- New weakness, numbness, trouble walking, or balance problems.
- Worsening shortness of breath, sudden chest symptoms, or severe pain not eased by meds.
- Increasing redness, swelling, drainage, or bleeding at an incision site.
Early reporting helps your team troubleshoot problems and preserve the benefits of therapy.
| Issue | What to look for | Action |
|---|---|---|
| Infection | Fever, redness, drainage | Call clinic; may need antibiotics or wound care |
| Lead or device problem | Sudden return of pain or odd sensations | Prompt evaluation; imaging or reprogramming may help |
| CSF leak | Positional headache, nausea | Contact surgeon right away for assessment |
Remember: serious complications are uncommon. Most problems can be fixed when reported early, helping maintain long‑term stimulation benefit and overall health.
Results, Success Rates, and Long‑Term Pain Management
After implantation, patients usually measure success by activity gains and fewer pain flares rather than a cure. Spinal cord stimulation aims to lower pain intensity and help you do more of the things you value.
What to expect: pain reduction vs. cure
The device rarely removes the root cause. Most people see meaningful pain relief that improves sleep, mood, and daily tasks.
Typical success benchmarks and factors that influence outcomes
Many programs define a successful trial as at least a 50% drop in symptoms. About half of implanted patients maintain that level of relief long term.
- Benchmarks: 50% pain reduction is a common target after a successful trial and implant.
- Key influences: diagnosis, pain distribution and quality, prior treatments, mental health, and following activity limits affect results.
- Programming matters: routine follow-up and reprogramming keep relief steady as routines change.
“Setting realistic goals before the trial helps you and your team measure meaningful improvements after the procedure.”
Some patients notice reduced benefit over years. When that happens, reprogramming or an updated device can restore coverage. Your surgeon and pain team will reassess options and adjust plans as needed.
Long-term approach: stay active within guidelines, address sleep or mood issues, and keep scheduled visits. These steps support durable pain management and better quality of life.
For a summarized review of outcomes and longer-term data, see this clinical review of stimulation outcomes.
Alternatives and Complementary Treatments to Cord Stimulation
Before any implant is considered, a range of conservative therapies are reviewed and optimized.
Non‑surgical and interventional options
Physical therapy and graded activity help rebuild strength and reduce pain with targeted exercises and pacing.
Medications like NSAIDs and select neuropathic agents can ease symptoms short term. Long‑term opioid therapy is usually avoided due to limited benefit and risks.
Targeted injections and nerve blocks may both diagnose and treat a specific source of pain without an implant.
Lifestyle, mental health, and when surgery is best
Weight management, sleep hygiene, and stress strategies often improve outcomes. Psychological support can strengthen coping and boost responses to treatment.
When imaging shows a correctable problem — such as nerve compression or instability — corrective surgery may offer the most direct relief.
“Combining therapies gives the best chance to reduce symptoms and delay or avoid more invasive procedures.”
| Approach | Role | When used |
|---|---|---|
| Physical therapy | Builds strength, mobility, graded activity | First‑line for chronic pain |
| Injections / nerve blocks | Diagnostic and therapeutic relief | When a specific pain generator is suspected |
| Medications | Symptom control; adjunctive care | Short to medium term or combined with PT |
| Surgery | Fixes structural problems like compression | If imaging and symptoms match a correctable lesion |
Positioning cord stimulation: it becomes an option when conservative care and, if appropriate, corrective surgery have not controlled symptoms adequately.
Conclusion
A short, monitored trial gives practical feedback about how much relief you may gain and helps guide the next steps.
strong, supportive team care frames the whole journey — from evaluation to a brief trial and, if helpful, a minimally invasive implant. The goal is to lower pain and improve daily function, not to promise a cure.
Your team stays engaged after the procedure for programming adjustments, wound checks, and long‑term management. Trials typically run about a week and most patients return home within one to two days after the implant.
Keep scheduled visits, follow activity limits, and reach out quickly with issues. If conservative treatments have not helped, ask your clinician whether an evaluation and a trial might be right for your situation and life goals.

