If constant discomfort has slowed your days, you are not alone. I have watched friends and family feel trapped by limits they never expected. That sense of lost normalcy is real and worth addressing with care and hope.
HF10 (HFX) offers a modern, non-drug option that uses 10-kHz high-frequency spinal cord stimulation to calm pain pathways. This approach is backed by large clinical trials and FDA labeling that highlights its superiority over older low-frequency systems.
The therapy is minimally invasive, trial-first, and fits daily life: it can run 24/7, has no tingling sensations for most users, and often needs little to no daily remote interaction. Many patients report better sleep, easier movement, and a clearer path back to routine activities.
Expect a patient-focused journey with quick recovery, insurance coverage in many cases, and ongoing support to optimize settings after implant. This page guides you through what spinal cord neuromodulation is, how 10-kHz therapy works, who may qualify, and how to begin.
Key Takeaways
- HF10 (HFX) delivers high-frequency spinal cord stimulation approved by the FDA.
- The system is minimally invasive and uses a trial-first approach.
- Many patients experience durable relief and improved daily function.
- It supports 24/7 use and does not cause typical tingling sensations.
- Coverage by Medicare and most insurers makes it an accessible option.
Lasting pain relief without major surgery or drugs
Many people find lasting relief without major surgery or daily medications through high-frequency neuromodulation. This drug-free approach lowers reliance on oral treatments that can cause side effects or dependence.
The procedure is minimally invasive, and most patients go home the same day. Compared with extensive spine surgery, recovery is quicker and day-to-day life resumes sooner.
Many experience meaningful improvement within days during a trial period. The trial-first model lets you test results before committing, so you can feel confident in your next step.
The system can be left on 24/7, providing steady relief and no restrictions on sleep. It is cleared for driving and designed to fit normal routines so people can keep their independence and enjoy better quality of life.
- Next steps in care: consultation, trial, then implant if the trial is successful.
- Our team helps verify coverage; Medicare and most private insurers commonly provide benefits.
What spinal cord stimulation is and how high‑frequency therapy works
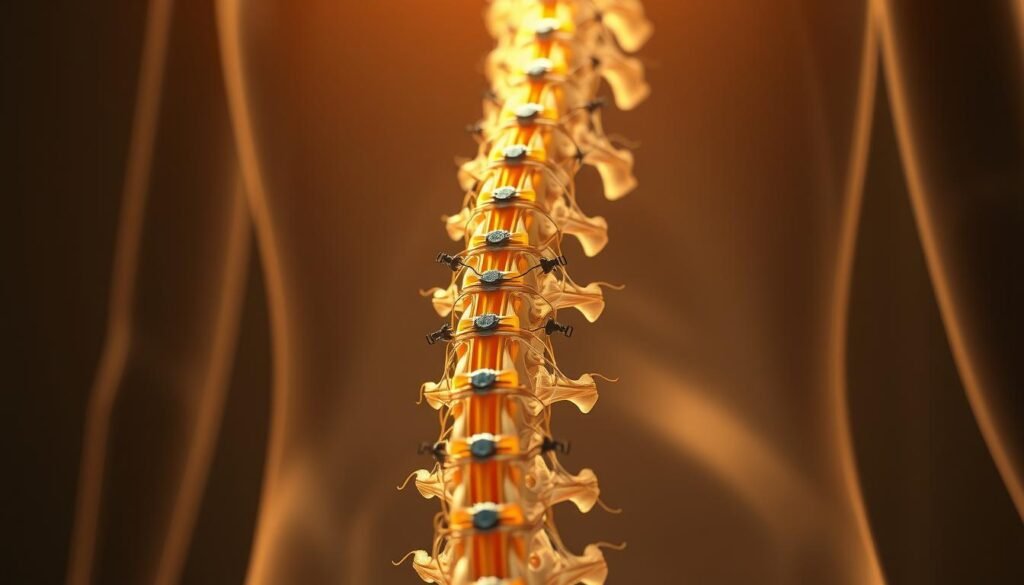
A small array of leads sits beside the spinal cord to alter overactive nerve signaling before it reaches the brain. Spinal cord stimulation places thin leads near the cord to modulate pathways and reduce the intensity of messages that travel to the brain.
Spinal cord stimulation basics: calming nerves and blocking pain signals to the brain
The system gently changes how nerves send signals so fewer strong messages reach the brain. SCS has been used in the United States for over 30 years and is a well‑understood option in chronic care.
How mild electrical pulses at 10 kHz differ from traditional low‑frequency SCS
High‑frequency 10‑kHz therapy delivers very mild electrical pulses that quiet overactive nerves rather than masking symptoms with buzzing. Clinical trials, including SENZA‑RCT, showed superior reductions in back and leg complaints at 12 and 24 months versus older low‑frequency devices.
Paresthesia‑free comfort: no tingling, just relief
This paresthesia‑free approach avoids the distracting tingling common with older systems. Because stimulation is gentle and consistent, many people report better sleep and less need to adjust settings during the day. The system is FDA approved for driving, reflecting steady, comfortable delivery without frequent interruptions.
- Targets signals at their source: reduces overall message volume to the brain.
- Improved function: helps sitting, standing, and walking feel easier.
- Modern safety: decades of SCS use updated with precise high‑frequency programming.
Nevro pain stimulator: what it is and why patients choose HFX/HF10
This next-generation system uses a small implanted generator and fine leads to provide round-the-clock high-frequency therapy near the spinal cord.
A small implantable device designed for chronic back and leg pain
HFX is a compact device placed under the skin with thin, flexible leads beside the cord. It delivers gentle 10‑kHz stimulation that many patients find comfortable and paresthesia-free.
The system is FDA approved with superiority labeling versus older spinal cord stimulator systems. It can stay on 24/7, requires little daily interaction, and is cleared for driving while active.
- Minimally invasive outpatient implant with same-day discharge.
- Programmed high-frequency stimulation that supports sleep, work, and errands.
- Customized follow-up programming to match changing needs.
| Feature | Benefit | Typical result |
|---|---|---|
| Small under-skin device | Discrete, low-profile wear | Normal clothing, daily activity |
| Thin flexible leads | Targeted cord stimulation | Improved back and leg function |
| 24/7 high-frequency delivery | Consistent relief without tingling | Better sleep and routine tasks |
Key benefits patients experience with Nevro HFX/HF10
Patients commonly report continuous symptom control that lets them move more and rest better. High‑frequency stimulation works day and night, so relief can be steady without the buzzing or interruptions some older systems cause.
Meaningful relief for chronic back and leg pain, day and night
Many people see true reductions in back and leg pain during a trial and after implant. Clinical evidence, including SENZA‑RCT, showed superior results at 12 and 24 months versus traditional systems.
Quality of life gains: sleep, mobility, and daily function
Better sleep continuity and easier walking or standing are common reports. Patients often say they have fewer interruptions in daily life and more ability to return to hobbies, work, and family duties.
FDA labeling advances: approved for driving and superior outcomes vs. traditional SCS
FDA superiority labeling and an approved-for-driving status reflect real-world benefits. The therapy is designed for 24/7 use, supports durable results, and often reduces reliance on oral medications and opioids.
For more on how this compares with older approaches, see the difference between traditional systems and HF10.
Conditions we treat with high‑frequency spinal cord stimulation
For many people, targeted high-frequency therapy offers relief when other treatments fail.
Primary indications include chronic back and leg conditions that persist despite medications, injections, or physical therapy. This option is often considered when conservative care has not brought lasting benefit.
Chronic back and leg symptoms, including non‑surgical refractory cases
HF10 has shown notable relief for chronic back and leg complaints, including cases where surgery is not planned or effective. Many patients report long-term improvement in daily function.
Painful diabetic neuropathy and long‑term nerve issues in the legs and feet
High-frequency cord stimulation can quiet overactive nerve signaling in the legs and feet. Clinical experience shows high responder rates and gains in walking tolerance, standing time, and balance for many patients.
- When to consider treatment: after medications, injections, or PT fail to deliver durable results.
- Personalized plan: a trial period verifies benefit before a permanent implant.
- Coordinated care: our team works with your specialists to integrate this therapy into ongoing care.
- Coverage: Medicare and most private insurers commonly provide benefits, easing access and affordability.
“Many patients report lasting relief and functional gains that let them return to daily activities with less interruption.”
| Condition | How HF10 helps | Typical patient result |
|---|---|---|
| Chronic back | Reduces overactive signaling along the spinal cord | Improved sitting, standing, and daily tasks |
| Leg pain and neuropathy | Calms long-term nerve signals in legs and feet | Better walking tolerance and balance |
| Non-surgical refractory back pain | Offers an alternative when surgery is not chosen | Durable symptom reduction and function gains |
Who is a good candidate for spinal cord stimulator treatment
When standard care no longer meets goals for mobility and sleep, selecting a trial-first neuromodulation option can provide real-world answers.
When conservative treatments fall short and a minimally invasive option fits
Patients who still have persistent chronic pain that limits daily function despite medications, injections, or physical therapy may be candidates.
Ideal candidates want a non-opioid option and prefer to test results before committing to a permanent device.
- Clinical and imaging evaluation supports targeting the cord for neuromodulation.
- People with neuropathic features, such as diabetic neuropathy, or non-surgical refractory back symptoms often respond well.
- The process includes medical history review, prior treatment checks, imaging, and clear goal-setting for function and comfort.
Expectations: realistic goals focus on meaningful reduction in pain intensity and improved ability to sit, stand, walk, and sleep.
Spinal cord stimulation complements multidisciplinary care. It does not replace essential medical management or reconditioning. Coverage by Medicare and most private insurers is common, and our team helps with pre-authorization to explore this option and potential pain relief.
The path to relief: trial period and minimally invasive implant procedure
A brief, monitored trial lets you experience therapy effects before any implant. Thin leads are placed and connected to an external unit so you can test real‑world relief over several days.
Temporary trial: feel the results in days before you decide
The trial uses an external power source so you can live normally while we track results. You and your clinician review scores for sleep, activity tolerance, and overall comfort to decide the next step.
Outpatient implant: thin leads near the spinal cord, small device under the skin
The implant procedure is minimally invasive and done with fluoroscopic guidance to place thin leads near the cord. A small generator sits under the skin and most patients go home the same day.
Living with the system: limited to no daily remote use, can be left on 24/7
High‑frequency therapy works through mild electrical pulses designed to quiet overactive pathways for steady comfort. The system typically needs little daily interaction and is designed for continuous use.
| Step | What to expect | Typical outcome |
|---|---|---|
| Trial (several days) | External unit with thin leads; log activity and scores | Measure relief and function before implant |
| Implant procedure | Outpatient, fluoroscopy-guided lead placement, small under-skin device | Same-day discharge and gradual return to light activity |
| Follow-up | Simple visits to fine-tune programming | Personalized settings for steady relief |
Proven results backed by clinical evidence
Large randomized and real-world studies document lasting gains in comfort and daily activity with modern cord stimulation.

SENZA‑RCT and 24‑month outcomes: superior relief for back and leg pain
The SENZA‑RCT (Kapural 2015; 2016) showed clear superiority at 12 and 24 months for back and leg pain and for functional scores compared with traditional low-frequency systems.
Real‑world results: improved function and durable relief over years
Multicenter registry reviews, including Stauss 2019, report durable benefit in routine practice. Many patients kept gains for months and years, reporting better sleep, walking, and standing.
Reduced opioid use: higher opioid‑free rates and lower doses over time
Studies also show an opioid-sparing effect. After high-frequency therapy, more patients become opioid-free and average daily doses drop for many who continue medications.
- Pivotal trial: SENZA‑RCT—superior back and leg results at 12 and 24 months.
- Function gains: improved sitting, walking, and sleep that mirror reduced symptom intensity.
- Real-world durability: multicenter data confirm benefit beyond the short term.
- Opioid reduction: higher opioid-free rates and lower average dosages after therapy.
“Randomized trials and large cohorts together support both efficacy and practicality for many patients.”
Individual results vary. A brief trial helps predict personal benefit before any permanent implant. Discuss expected outcomes with your clinician based on diagnosis and goals.
Safety, recovery, and what to expect over the first weeks and months
In the weeks after implant, attention to wound care and activity limits guides a safe recovery. Most patients go home the same day and begin simple self‑care right away.
Common, rare risks, and how we minimize complications
Common effects include temporary soreness, swelling, or tenderness at the incision sites. These typically ease with rest, ice, and standard wound care.
Rare risks can include lead migration, loss of relief, or allergic reaction. We reduce these risks with careful placement, secure anchoring, and scheduled follow‑ups to detect issues early.
“Early checks and timely programming adjustments keep recovery on track and lower the chance of avoidable problems.”
Recovery timeline, activity guidelines, and long‑term device care
Typical timeline: expect about 6 to 8 weeks for initial healing. Heavy lifting and bending are limited during this time to protect the cord leads.
- Return home same day and rest for the first 48–72 hours.
- Gradual increase in activity over several weeks per your clinician’s plan.
- Follow-up visits fine‑tune programming as your activity level rises over the first months.
Good wound care, movement precautions, and open communication with your care team are key to steady recovery. The therapy aims to deliver sustained pain relief without cognitive or bowel side effects linked to many medications.
| Stage | What to expect | Patient action |
|---|---|---|
| 0–72 hours | Soreness, dressing in place | Rest, icing, keep dressing clean |
| 2–6 weeks | Slow activity increase; avoid heavy lifting | Follow activity limits; attend programming visit |
| 6–8+ weeks | Most healing complete; resume normal tasks | Maintain wound checks; report unusual symptoms |
Coverage, costs, and access across the United States
Access to high‑frequency HF10 therapy is available nationwide for people who meet clinical criteria. Medicare and nearly all private insurers cover this treatment, and our team helps verify benefits and submit prior authorizations.
Insurance and Medicare coverage
Most plans recognize HF10 as a standard of care for appropriate candidates. That means patients often face only plan-specific deductibles and copays rather than full device costs.
We review your policy, explain expected out‑of‑pocket costs, and outline any device-related coverage details so there are no surprises.
Scheduling your consultation and trial
At your consultation, we perform a medical review, assess candidacy, and discuss logistics. If appropriate, we schedule a short trial so patients can try the device before implant.
- Stepwise care: consult → insurance check → trial → outpatient implant for responders.
- Convenience: 24/7 therapy, FDA approved for driving, and minimal daily interaction.
- Bring to your visit: goals, questions, and current medication list to maximize the appointment.
“Start with a consultation to confirm coverage and set realistic goals for relief.”
Ready to explore options? Contact our scheduling team to verify benefits and book a consultation so you can decide with confidence.
Conclusion
This therapy delivers continuous 10‑kHz stimulation to quiet overactive nerves and reduce disruptive signals to the brain. It is a modern spinal cord stimulator option that often gives steady, paresthesia‑free relief day and night.
The treatment is minimally invasive and suits people with chronic back and leg conditions who want to avoid or delay major surgery. A brief, reversible trial lets each patient test real-world results before a permanent implant.
Clinical data show superior outcomes at 12 and 24 months, durable gains over years, and reduced opioid reliance. Practical benefits include better sleep, easier mobility, and the ability to drive with confidence.
Ready to learn more? Schedule a consultation so our team can review your options, verify coverage, and walk you through the trial and procedure. See what conditions spinal cord stimulators can treat to decide if this treatment fits your goals.

