In America, someone has spinal surgery every 30 seconds hoping to stop chronic pain. But, 40% of these patients keep feeling pain even after surgery. This has led to the search for new ways to manage chronic pain.
Spinal Cord Stimulation is a big step forward in treating pain. It started in the late 1960s. It uses electrical pulses to block pain signals before they hit the brain. It’s like a pacemaker but for the nervous system.
For the 50 million Americans with chronic pain, this therapy offers hope. It works when other treatments don’t. The conditions it can treat include back pain and nerve disorders.
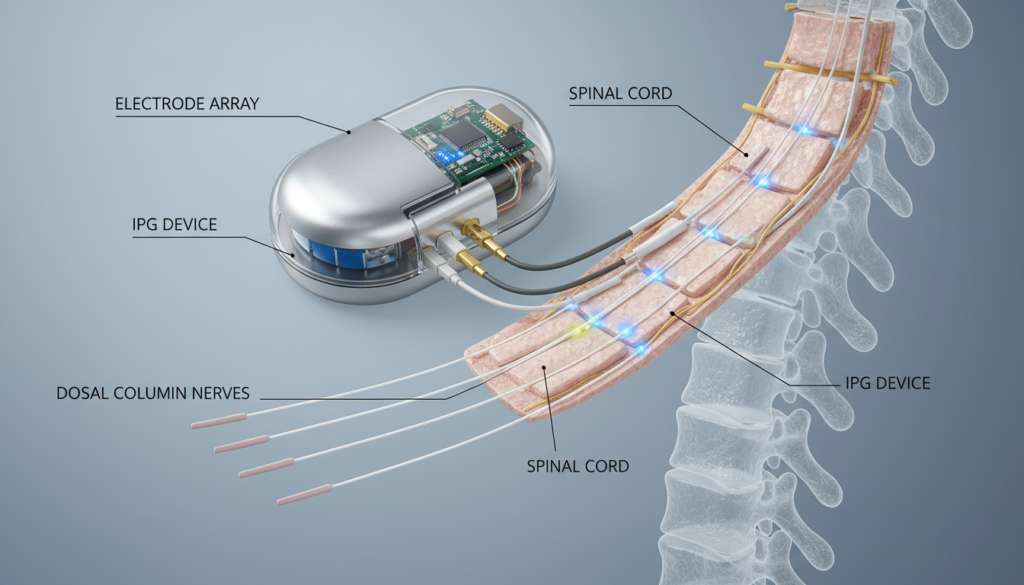
Today, we use tiny electrodes near the spine for this therapy. They connect to a small device under the skin. This device sends electrical impulses to change pain messages in the spinal cord.
Patients can adjust the settings with a remote. This lets them control their pain relief all day.
Key Takeaways
- Spinal Cord Stimulation blocks pain signals before they reach the brain using electrical impulses
- The therapy helps 50-70% of patients achieve significant pain reduction
- Chronic pain management through this method reduces dependency on opioid medications
- The procedure is reversible and adjustable based on patient needs
- Neurostimulation therapy treats conditions like Failed Back Surgery Syndrome and Complex Regional Pain Syndrome
- Patients control their pain relief levels with a handheld remote device
What is Spinal Cord Stimulation?
Spinal cord stimulation is a new way to manage chronic pain. It has helped thousands of people take back their lives. This treatment uses advanced tech to stop pain signals before they reach the brain.
Definition and Overview
Spinal cord implants are small devices placed near the spine. They send mild electrical pulses to certain nerve fibers. These neuromodulation devices create an electrical field that blocks pain messages.
Instead of pain, many feel a mild tingling called paresthesia. Newer systems can even offer relief without any sensation.
The system has three main parts:
- Thin wire electrodes in the epidural space
- A battery-powered pulse generator (like a pacemaker)
- A remote control for adjusting settings
How It Works
The science behind it is based on gate control theory. This theory was developed by Ronald Melzack and Patrick Wall in 1965. It says that non-painful input can block pain signals from reaching the brain.
The device stimulates large nerve fibers that carry touch sensations. This overpowers the smaller fibers that send pain signals.
Recent studies show spinal cord implants do more than block signals. They also change the spinal cord’s chemistry. They increase good substances like GABA and serotonin while reducing pain-causing chemicals like glutamate. This makes implantable pain relief very effective for some chronic pain conditions.
Conditions Treated by Spinal Cord Stimulation
A spinal cord modulator offers hope for those with chronic pain that hasn’t been helped by other treatments. This technology targets specific pain conditions, mainly those caused by damaged or misfiring nerves. Doctors carefully check each patient to see if dorsal column stimulation can help.
Chronic Pain Syndromes
Chronic pain affects millions in the U.S. and can last for years. Spinal cord stimulation helps with several chronic pain syndromes, like post-laminectomy syndrome and arachnoiditis. It’s most effective for pain that travels along nerve paths, not just muscle or joint pain.
Neuropathic Pain Conditions
Spinal cord stimulation is very effective for neuropathic pain. It works well for diabetic neuropathy and peripheral neuropathy. The electrical impulses stop pain signals before they reach the brain, giving relief without harsh meds. Studies show it helps patients with nerve pain function better every day.
Failed Back Surgery Syndrome
Failed Back Surgery Syndrome affects up to 40% of those who have had spinal surgery. It causes ongoing pain despite surgery. Studies show spinal cord modulators are more effective than traditional pain management for these patients.
Complex Regional Pain Syndrome
Complex Regional Pain Syndrome causes intense burning pain, usually in an arm or leg. Dorsal column stimulation is a top treatment for this condition. Patients often see a big drop in pain and regain function after getting the implant.
The Mechanism of Action
To understand Spinal Cord Stimulation, we must look at how pain signals travel through our nervous system. This therapy blocks pain messages before they reach the brain. It helps those with chronic pain manage their symptoms better.
Pain Pathways and Nerve Signals
Pain starts when nerve endings detect harm, like extreme heat or pressure. Different nerves carry pain signals at different speeds. Thin nerves send slow pain, while thicker ones handle touch and pressure.
These nerves meet at the spinal cord’s dorsal horn. There, they connect with neurons that send messages to the brain through the spinothalamic tract.
The Role of Electrical Stimulation
Spinal Cord Stimulation devices send mild electrical pulses to the spinal cord. These pulses activate large nerve fibers. This triggers cells to release chemicals like GABA and glycine.
These chemicals block pain signals from going up to the brain. It’s like closing a gate before the pain reaches us.
| Nerve Fiber Type | Function | Response to Stimulation |
|---|---|---|
| A-beta fibers | Touch and pressure | Activated by device |
| C fibers | Slow pain signals | Blocked by stimulation |
| A-delta fibers | Fast pain signals | Suppressed by gate control |
This therapy can feel like a gentle tingling or work below our awareness. It replaces painful feelings with more bearable ones. For conditions with poor blood flow, it helps manage pain by improving oxygen to tissues.
Types of Spinal Cord Stimulators
Spinal cord implants come in different designs, each with its own benefits for pain relief. The best choice depends on your pain, lifestyle, and medical history. Today, you can find simple systems and advanced ones with complex programming.
Fully Implantable vs. Partially Implantable
Fully implantable systems have everything under the skin, including the battery. They are more convenient and lower the risk of infection. You can swim, bathe, and do activities without worry.
Partially implantable systems have an external power source. They are less common but good for those who need more time to try it out or don’t want surgery for battery replacement. You can change settings easily with the external control.
Dual-Channel Systems
Dual-channel systems can stimulate two spinal areas at once. They are great for complex pain in different parts, like both legs or the back and leg. Each channel can be set up differently for the best pain relief.
New Innovations in Technology
New tech includes closed-loop systems that adjust on their own. They change based on your body’s position and movement. These smart implants avoid the tingling feeling of older devices.
Now, batteries can last up to 10 years, cutting down on surgeries. Devices from Abbott, Boston Scientific, and Medtronic are safe for MRI scans. This lets patients get important tests done without worry.
Benefits of Spinal Cord Stimulation
Living with chronic pain can change your life a lot. A spinal cord modulator can help you feel better and live more freely. It’s a new way to treat pain that does more than just ease discomfort.
Pain Relief and Quality of Life
People who try dorsal column stimulation often see big changes in their pain. They might feel up to 81% less pain. This lets them do things they love again.
This therapy also helps in many ways:
- Better sleep and less tiredness
- Improved mood and mental health
- More mobility and physical strength
- More fun in social activities
Reduced Need for Pain Medications
This treatment can also help you use less pain medicine. This is good because it means less risk of side effects and addiction. It’s a safe, drug-free way to manage pain.
Minimally Invasive Nature
Dorsal column stimulation is less invasive than big surgeries. It only needs small cuts. This means you can recover quickly and might even go home the same day.
Studies show that quality-of-life scores improve a lot with this therapy. It’s a smart choice compared to many surgeries or long-term medication.
Potential Risks and Complications
Spinal Cord Stimulation can greatly help with chronic pain. But, it’s important to know the possible risks before starting. Most problems are rare and can be avoided with good medical care. Your doctor will check your situation to lower any risks.
Surgical Risks
The surgery to implant the device has common risks. About 3-4% of patients get an infection at the site, as reported by the Journal of Neurosurgery. Bleeding or nerve damage can happen during the procedure. Some might get spinal fluid leaks, but these usually get better with simple treatment.
Some conditions make surgery too risky. These include infections near the site, unusual spine shapes, and bleeding problems. People taking blood thinners need careful management to avoid complications.

Device Malfunction
Over time, the device might have technical problems. About 13% of patients experience lead migration, which means the electrodes move. This can lead to less pain relief or odd feelings. Battery failure or programming errors might need more surgery to fix.
Long-term Risks
Using Spinal Cord Stimulation for a long time has its own challenges. Studies show it helps some pain more than others. Scar tissue around the leads can make it less effective over time. Regular check-ups are key to catching and fixing these problems early.
Who is a Candidate for Spinal Cord Stimulation?
Not everyone with chronic pain can get spinal cord implants. Doctors check each patient to see if this device will help. They look at medical criteria and test patients to find the best results.
Eligibility Criteria
Patients for implantable pain relief must meet certain criteria. Their pain must last at least six months, even after trying many treatments. These treatments often include physical therapy, medicines, nerve blocks, and sometimes surgery.
The pain cannot be fixed with regular surgery. Mental health is also important. Patients get checked for depression or anxiety that might affect treatment success. Studies show that mental health issues can lead to poor results with spinal cord implants.
Evaluation Process
The first step is a trial with a temporary device. Patients need to see at least 50% pain reduction to get a permanent implant. Research with 318 patients showed that 61% got significant relief during the trial.
| Evaluation Step | Purpose | Success Indicator |
|---|---|---|
| Medical History Review | Confirm chronic pain duration | 6+ months documented pain |
| Psychological Assessment | Screen mental health status | No severe untreated conditions |
| Trial Stimulation | Test device effectiveness | 50% or greater pain reduction |
Age, pain intensity, and how long the pain lasts don’t really affect success. Each case is looked at based on health and pain patterns.
The Spinal Cord Stimulation Procedure
The journey to pain relief starts with a trial period. This helps figure out if the treatment will work for you. The process includes careful preparation, precise surgery, and follow-up care for the best results.
Pre-Procedure Preparation
Your pain specialist will do a detailed check before the trial starts. The trial begins with temporary leads in the epidural space. This is done under local anesthesia and mild sedation to keep you relaxed.
The temporary leads connect to an external generator. You’ll wear this on your belt or shoulder for about a week. During the trial, you’ll do your usual activities and track your pain and life improvements. Your team looks for at least 50% pain reduction to call the trial a success.
The Implantation Process
If the trial is successful, the permanent implantation comes next. The surgeon makes a small cut and uses fluoroscopy to place the electrodes. The pulse generator is implanted under the skin, usually in the buttock or abdomen.
Most patients have this procedure as outpatients and go home the same day.
Recovery and Follow-Up Care
Recovery means some soreness and tiredness for a few days. You should do light activities but avoid hard movements and bending for weeks. Your pain specialist will see you regularly to adjust the device settings.
Long-term care includes check-ups for adjustments and wireless charging when needed.
Effectiveness and Success Rates
Studies on Spinal Cord Stimulation show it’s helping many with chronic pain. Clinical trials and patient stories highlight its benefits. Recent studies show it can reduce pain and improve life quality for a long time.
Clinical Outcomes
A 2024 study found Spinal Cord Stimulation beats traditional pain treatments. Most patients see big pain drops in six months. It works best for certain pain types.
| Condition | Pain Reduction Rate | Evidence Level |
|---|---|---|
| Failed Back Surgery Syndrome | 60-70% | Level A |
| Complex Regional Pain Syndrome (without allodynia) | 81% | Level A |
| Complex Regional Pain Syndrome (with allodynia) | 31% | Level B |
| Peripheral Neuropathy | 65-75% | Level A |
| Angina Pectoris | 70-80% | Level A |

Most patients see big life quality boosts. EQ-5D assessments show better daily life and less disability. Newer stimulation methods work even better than old ones.
Long-term Studies
Long-term studies show Spinal Cord Stimulation keeps working for years. Devices last 5 to 10 years, depending on use. Studies confirm pain relief stays strong over time.
Regular check-ups and adjustments keep treatment effective. This ensures long-term pain management success.
Alternative Pain Management Approaches
Before looking into spinal cord implants, patients try many pain management methods. Each method has its own benefits and works in different ways for different pain types. Knowing about these options helps patients choose the best treatment for them, even if traditional methods don’t work well.
Physical Therapy
Physical therapy helps build strength and improve movement with special exercises. Therapists create plans that focus on specific pain areas and movement issues. Regular therapy can lessen inflammation, boost flexibility, and strengthen muscles around painful spots.
Many find that physical therapy helps them avoid needing implantable pain devices. It tackles the mechanical problems that cause pain.
Medication Management
Pain meds range from simple anti-inflammatories to stronger prescription drugs. Doctors carefully pick the right meds and amounts to control pain without too many side effects. NSAIDs like ibuprofen fight inflammation, while stronger opioids tackle severe pain. Gabapentin works differently, targeting nerve pain.
Some use creams or patches that apply medication directly to pain spots. This way, they avoid the whole-body effects of pills.
Psychological Support
Cognitive behavioral therapy teaches patients to cope with pain and change how they see it. Mental health experts teach relaxation, mindfulness, and stress management. These skills can lower pain levels.
Depression and anxiety often go with chronic pain, making mental support key. Patients learn to spot pain triggers and respond in healthy ways. A positive mindset is key for those thinking about a neuromodulation device, as it affects treatment success.
Patient Experiences and Testimonials
Real patients who got spinal cord modulator implants share amazing stories. They talk about going from constant pain to feeling free again. Their stories show how this treatment can change lives and the hard work needed for success.
Real-Life Success Stories
Many say dorsal column stimulation changed their lives. A woman from Texas had back pain for eight years. But with the spinal cord modulator, she could garden and play with her grandkids again.
A man from Ohio, who used to work in construction, could sleep through the night for the first time in five years. These stories show how this treatment can improve lives.
Success rates vary, but those who get involved in their treatment do best. This means going to programming sessions, keeping the device in good shape, and following doctor’s orders. Being able to adjust the settings helps patients manage their pain better, fitting relief to their daily activities.
Common Concerns and Hurdles
New patients often worry about keeping the device working and changing their lifestyle. The first few weeks can be tough as the body gets used to the stimulation. Some find the tingling strange at first, but most get used to it in a few weeks.
Charging the device weekly, for 30-60 minutes, becomes a regular task. Patients also learn to deal with airport security and MRI rules. Having support from friends and family, and being financially stable, helps a lot in getting good results from this advanced pain treatment.
Insurance and Cost Considerations
Understanding the costs of Spinal Cord Stimulation is key for patients. Insurance coverage and costs differ, but knowing what to expect helps. This knowledge makes planning for chronic pain treatment easier.
Coverage Options
Major insurance providers, including Medicare and Medicaid, often cover Spinal Cord Stimulation. They require certain criteria to be met. This includes:
- Documentation of chronic pain lasting at least six months
- Evidence of failed conservative treatments (physical therapy, medications, injections)
- Successful completion of a trial stimulation period
- Psychological evaluation clearance
Private insurers like Anthem, Aetna, and UnitedHealthcare have their own approval processes. It’s best to contact your insurance provider directly. The trial phase serves a dual purpose – it proves effectiveness and meets insurance requirements.
Cost Breakdown of Procedure
The cost of neurostimulation therapy includes several parts. Without insurance, it can cost between $30,000 and $50,000. With insurance, patients usually pay:
| Cost Component | Typical Range |
|---|---|
| Deductible | $500 – $5,000 |
| Copayment (10-20%) | $3,000 – $10,000 |
| Annual Device Maintenance | $200 – $500 |
| Battery Replacement (non-rechargeable) | $5,000 – $15,000 every 3-5 years |
Rechargeable systems cost more upfront but save money over time. They avoid the need for battery replacement surgeries. Many hospitals offer financial counseling to help with payments and insurance appeals for chronic pain treatments.
Ongoing Research and Developments
The field of spinal cord implants is growing fast. Scientists and engineers are working hard to make better pain relief devices. These new technologies could change how we manage pain, making it more effective.
Emerging Technologies in Spinal Cord Stimulation
New breakthroughs include high-frequency stimulation and burst waveform patterns. These help patients feel less pain without the usual tingling. Closed-loop feedback systems are also a big step forward. They adjust the treatment based on how the nerves are working.
Now, more devices can handle MRI scans safely. Most can handle 1.5 Tesla scans. Some can even handle 3.0 Tesla scans, but with special safety steps.
| Technology Type | Key Benefits | Availability |
|---|---|---|
| High-Frequency Stimulation | No tingling sensation | Currently available |
| Burst Waveforms | Better pain coverage | Currently available |
| AI-Powered Programming | Automated optimization | In development |
| Biocompatible Materials | Reduced tissue reaction | Testing phase |
Future Directions for Pain Management
Artificial intelligence is a big part of the future of spinal cord implants. These AI systems will learn from patients and adjust treatments for better results. New materials are being made to help the body accept implants better. Also, researchers are working on devices that can last over 15 years without needing a new battery.
Conclusion: Is Spinal Cord Stimulation Right for You?
Spinal cord stimulation has become a key treatment for chronic pain. It uses dorsal column stimulation to block pain signals. Before trying it, think about your pain, medical history, and what you hope to achieve.
Many find it helps when other treatments fail. It’s a chance to find relief.
Weighing the Pros and Cons
Spinal cord stimulation can greatly reduce pain and lower the need for pain meds. People often sleep better, move more, and feel happier. It’s also safe to turn off or remove if needed.
But, there are risks like surgery complications and regular check-ups. It’s important to weigh these against the benefits.
Next Steps for Interested Patients
If you’re thinking about dorsal column stimulation, talk to a pain management specialist. Places like Cleveland Clinic or Mayo Clinic are good choices. They’ll check if you’re a good fit for this treatment.
They’ll look at your medical history, do tests, and check your mental health. Your doctor will explain the trial, what to expect, and if it’s right for you.

