Chronic pain in the chest and upper abdomen can be debilitating, affecting every aspect of a person’s life. For those suffering from persistent pain that hasn’t responded to conventional treatments, there’s hope in a specialized medical procedure known as an intercostal nerve block.
This procedure involves injecting medication under the ribs to target specific nerves that transmit pain signals, providing relief for conditions such as postherpetic neuralgia, rib fractures, and chest surgeries.
Understanding intercostal nerve blocks is crucial for patients seeking alternative solutions for managing their pain. This article will cover the procedure, conditions treated, benefits, risks, and expected outcomes, offering a comprehensive overview for those seeking pain relief.
Key Takeaways
- Intercostal nerve blocks are a specialized procedure for managing chronic pain in the chest and upper abdomen.
- The procedure targets specific nerves to interrupt pain signals.
- It is used to treat conditions such as postherpetic neuralgia, rib fractures, and post-surgical pain.
- Performed by specialized pain management physicians.
- Can significantly improve quality of life for many patients.
Understanding Intercostal Nerves and Pain
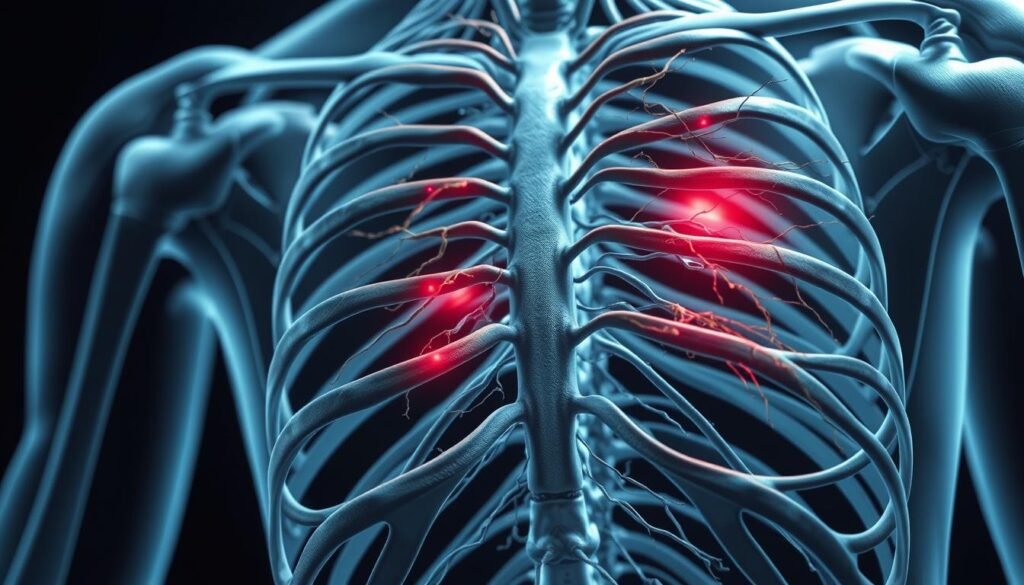
Intercostal nerves play a crucial role in our nervous system, and understanding their function is key to addressing related pain issues. These nerves run between the ribs and are responsible for transmitting pain signals.
What Are Intercostal Nerves?
Intercostal nerves are a vital part of the nervous system, providing sensation to the chest and abdominal areas. They are located between the ribs and play a crucial role in controlling muscles and transmitting sensory information from the skin and muscles in the chest and abdominal wall.
How Intercostal Neuralgia Develops
When one of these nerves or the tissue around them becomes irritated or inflamed, it can cause pain. This condition is known as intercostal neuralgia, characterized by a band-like pain that wraps around the chest or abdomen. The pain can be constant or intermittent and may worsen with movements like coughing or sneezing. For more information on managing nerve-related pain, visit this resource.
| Causes of Intercostal Neuralgia | Symptoms |
|---|---|
| Trauma, Surgery, Infection | Sharp, Shooting Pain, Burning Sensations |
| Inflammation, Compression | Tingling, Numbness, Hypersensitivity |
The Intercostal Nerve Block Procedure
The intercostal nerve block procedure is a valuable tool for diagnosing and treating pain. It involves the injection of medication into or around the intercostal nerves to block pain signals to the brain.
Definition and Purpose
An intercostal nerve block is a procedure that involves injecting a local anesthetic or a corticosteroid into the intercostal nerves. The primary purpose of this block is to provide pain relief by interrupting the pain signals transmitted to the brain. It is used both as a diagnostic tool to identify the source of pain and as a therapeutic measure to manage pain.
Types of Nerve Blocks
There are several types of nerve blocks available for managing intercostal neuralgia. These include:
- Diagnostic blocks: Temporary injections used to confirm the source of pain.
- Therapeutic blocks: Use local anesthetic combined with corticosteroids for longer-lasting pain relief.
- Neurolytic blocks: Intentionally damage the nerve to provide more permanent relief for severe pain.
- Continuous nerve blocks: Use catheters to deliver medication over an extended period, often for post-surgical pain relief.
The choice of block type depends on the patient’s specific condition and pain severity. Advances in imaging technology have improved the precision and safety of these procedures.
Conditions Treated with Intercostal Nerve Blocks
The application of intercostal nerve blocks extends to several painful conditions that affect the chest and abdominal regions. These blocks are particularly useful for managing pain that is resistant to other treatments.
Post-Surgical Pain Management
Intercostal nerve blocks are effective in managing pain after surgical procedures. By blocking the nerve signals, these injections can significantly reduce discomfort and improve patient outcomes.
Rib Fractures and Trauma
In cases of rib fractures or trauma, intercostal nerve blocks can provide substantial relief. The procedure helps in reducing the pain associated with such injuries, facilitating easier breathing and movement.
Shingles and Postherpetic Neuralgia
The herpes zoster virus, which causes shingles, can lead to postherpetic neuralgia, a condition characterized by persistent neuralgia. Intercostal nerve blocks can help manage this condition by interrupting pain signals. According to a study, “Early intervention with nerve blocks during shingles may reduce the risk of developing postherpetic neuralgia.” The procedure can also help patients who develop allodynia, a condition where even light touch to the skin causes pain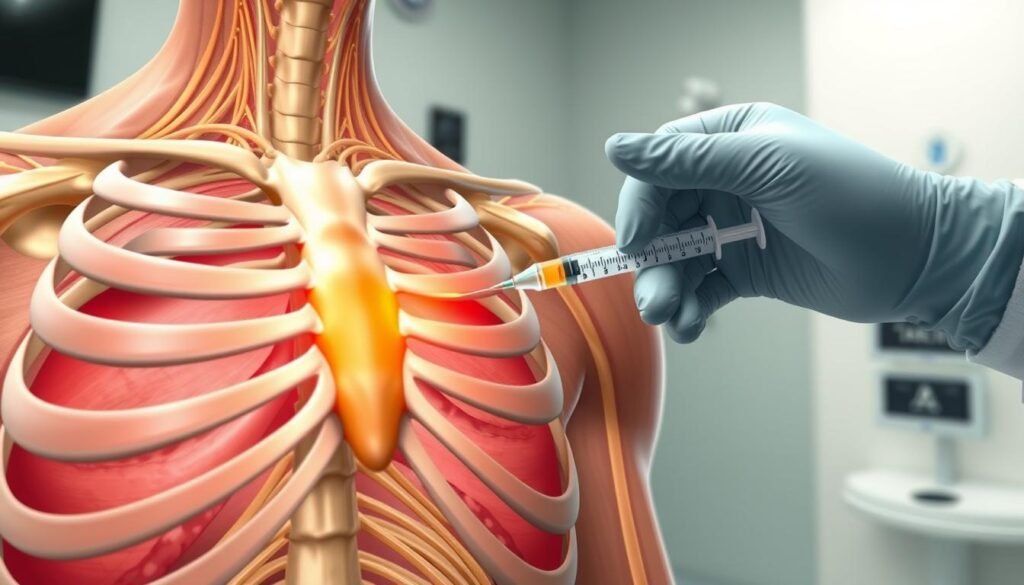
How an Intercostal Nerve Block Works
To understand how an intercostal nerve block works, it’s essential to grasp the basics of the procedure and its effects on the body. An intercostal nerve block is a procedure that involves injecting medication into the nerves surrounding the ribs to alleviate pain.
Mechanism of Action
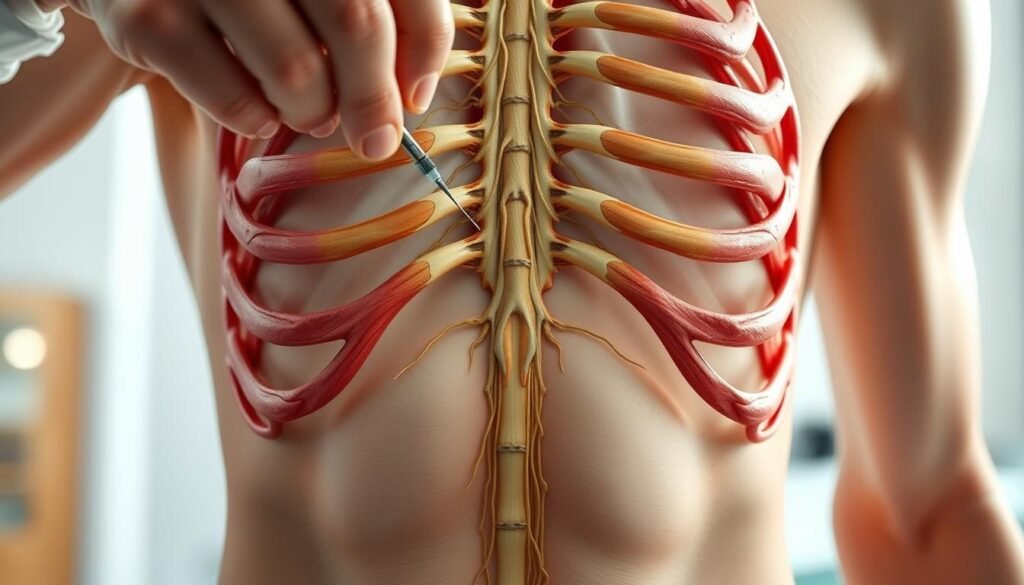
The intercostal nerve block works by injecting a local anesthetic and a steroid into the area around the nerve causing the pain. This injection helps to reduce inflammation and numb the pain. The needle is carefully inserted between two ribs to deliver the medication directly to the affected area.
Step-by-Step Process
The procedure begins with the patient positioned on their side or face down. The site of the injection is cleaned and sterilized to prevent infection. Using imaging guidance, such as fluoroscopy or ultrasound, the physician ensures precise needle placement near the target nerve. A local anesthetic is administered to the skin and superficial tissues before the deeper injection. The entire procedure typically takes 15-30 minutes. After the injection, the patient is monitored for any immediate side effects before being discharged.
Ideal Candidates for Intercostal Nerve Blocks
Determining the ideal candidate for an intercostal nerve block involves a comprehensive evaluation of the patient’s medical history and current condition. This procedure is typically considered for individuals suffering from chronic pain that has not responded to other treatments.
Who Can Benefit Most
Patients who can benefit most from intercostal nerve blocks are those with conditions such as post-surgical pain, rib fractures, shingles, or postherpetic neuralgia. These conditions often result in significant pain that can be challenging to manage with conventional treatments.
- Patients with bleeding disorders or those taking anticoagulant medications require careful consideration.
- Allergies to local anesthetic or other medications used during the procedure must be disclosed.
Pre-Procedure Considerations
Before undergoing an intercostal nerve block, several factors are evaluated. A thorough physical examination and review of imaging studies are conducted to determine the appropriate level for the injection.
- Patients are advised on which medications to continue or discontinue before the procedure.
- Informed consent is obtained, ensuring patients understand the benefits, risks, and alternatives.
- Arrangements for transportation home are recommended, as driving is not advised immediately after the nerve block.
Benefits and Effectiveness
Intercostal nerve blocks have emerged as a highly effective treatment for various chronic pain conditions. These blocks offer significant benefits to patients suffering from intercostal neuralgia and other related conditions.
Pain Relief Duration
The duration of pain relief from intercostal nerve blocks can vary significantly among patients. Some individuals may experience relief for several months, while others may require repeated injections to maintain the effect. Factors influencing the duration include the underlying cause of pain, the severity of the condition, and individual patient response.
Improved Quality of Life
Effective pain relief from intercostal nerve blocks can significantly enhance patients’ overall quality of life. The benefits include:
- Improved ability to engage in physical therapy and rehabilitation programs
- Enhanced respiratory function, particularly for patients with rib fractures or thoracic surgery
- Better sleep quality, leading to improved overall well-being
- Reduced anxiety and depression associated with chronic pain
- Increased ability to perform daily activities and return to work or hobbies
By reducing reliance on oral pain medications, intercostal nerve blocks can also decrease side effects and improve cognitive function.
Potential Risks and Side Effects
It’s essential to understand the potential risks and side effects associated with intercostal nerve blocks. While generally considered safe, the procedure can have complications.
Common Side Effects
Common side effects of intercostal nerve blocks may include temporary numbness or weakness in the chest area, which typically resolves on its own within a few hours. Some patients may experience discomfort or pain at the injection site, which can be managed with over-the-counter pain medications. In rare cases, patients may experience an allergic reaction to the medications used.
When to Contact Your Doctor
It’s crucial to seek medical attention if you experience any severe symptoms after an intercostal nerve block. Warning signs include difficulty breathing, chest pain, or shortness of breath, which could indicate a pneumothorax. Other concerning symptoms are fever, increasing pain, redness, swelling, or discharge at the injection site, which may indicate an infection. Additionally, persistent numbness or weakness lasting more than 24 hours, severe headache, or signs of allergic reactions should be reported to your doctor.
Conclusion
The use of intercostal nerve blocks has emerged as an effective intervention for several types of chest and upper abdominal pain. This procedure is particularly valuable for managing post-surgical pain, rib fractures, shingles, and intercostal neuralgia. While results can vary between patients, many experience significant pain relief and improved quality of life following the nerve block procedure.
It’s essential to note that intercostal nerve blocks are typically part of a comprehensive pain management approach. According to a study published on the National Center for Biotechnology Information website (https://pmc.ncbi.nlm.nih.gov/articles/PMC5292853/), proper patient selection and technique are crucial to maximize benefits and minimize risks. Patients experiencing chronic chest wall or upper abdominal pain are encouraged to discuss this option with their healthcare providers.
Advancements in imaging guidance continue to improve the safety and efficacy of intercostal nerve blocks. Open communication with healthcare providers about expectations, concerns, and outcomes is essential for optimal pain management. For many patients suffering from intercostal nerve pain, these blocks offer a valuable option for reclaiming comfort and function in their daily lives.

