Chronic headaches can be debilitating, affecting daily life and overall well-being. For those suffering from persistent head pain, an occipital nerve block can be a game-changer. This procedure involves injecting a combination of pain medicine and steroids into the scalp at the back of the head, providing quick relief from chronic headaches caused by irritation to the nerves in this area.
The nerve block is a minimally invasive treatment option that targets the root cause of the pain, offering a promising solution for those seeking relief from chronic head and neck pain.
Key Takeaways
- An occipital nerve block is a procedure that injects pain medicine and steroids into the scalp.
- This treatment targets chronic headaches caused by nerve irritation.
- The nerve block is a minimally invasive procedure.
- It provides quick relief from chronic head and neck pain.
- Patients suffering from various headache disorders may benefit from this treatment option.
What Are Occipital Nerve Blocks?

The occipital nerve block is a procedure that targets the occipital nerves at the base of the skull. These nerves are responsible for sensation in the scalp, and the procedure involves injecting a combination of local anesthetic and anti-inflammatory medications to provide pain relief.
Definition and Purpose
Occipital nerve blocks are specialized medical interventions designed to alleviate pain in the scalp by targeting the occipital nerves. The primary purpose of these blocks is to interrupt pain signals transmitted through these nerves, providing relief for patients suffering from various headache disorders and cervical pain conditions.
The procedure involves injecting a combination of local anesthetic and anti-inflammatory medications around the affected occipital nerves, serving both diagnostic and therapeutic purposes.
Types of Occipital Nerves
There are three main types of occipital nerves that may be targeted during an occipital nerve block procedure: the greater occipital nerve, the lesser occipital nerve, and the third occipital nerve. Each of these nerves innervates different areas of the scalp, and understanding their roles is crucial for effective treatment.
The greater occipital nerve provides sensation to the majority of the posterior scalp, while the lesser occipital nerve supplies the lateral areas of the posterior scalp. The third occipital nerve innervates the lower occipital region, and targeting these nerves can provide significant pain relief for patients.
Anatomy of Occipital Nerves
Understanding the anatomy of the occipital nerves is crucial for diagnosing and treating various headache disorders. The occipital nerves are a group of nerves that provide sensation to the scalp.
Greater Occipital Nerve
The greater occipital nerve (GON) is the largest of the occipital nerves, originating from the C2 spinal nerve. It emerges between the obliquus capitis inferior and semispinalis capitis muscles before ascending to innervate the posterior scalp. The GON provides sensory innervation to approximately two-thirds of the posterior scalp.
Lesser Occipital Nerve
The lesser occipital nerve derives from the C2 and sometimes C3 spinal nerves. It courses laterally to the greater occipital nerve, supplying sensation to the lateral aspects of the occipital region and the posterior aspect of the ear.
Third Occipital Nerve
The third occipital nerve, the smallest of the three, originates from the C3 spinal nerve. It innervates the lower occipital region and upper cervical area, playing a significant role in cervicogenic headaches.
| Nerve | Origin | Innervation Area |
|---|---|---|
| Greater Occipital Nerve (GON) | C2 spinal nerve | Posterior scalp |
| Lesser Occipital Nerve | C2 and sometimes C3 spinal nerves | Lateral occipital region and posterior ear |
| Third Occipital Nerve | C3 spinal nerve | Lower occipital region and upper cervical area |
Conditions Treated with Occipital Nerve Blocks
Various headache conditions can benefit from the analgesic effects of occipital nerve blocks. These blocks are particularly useful in managing different types of head pain, providing relief for patients suffering from chronic headache disorders.
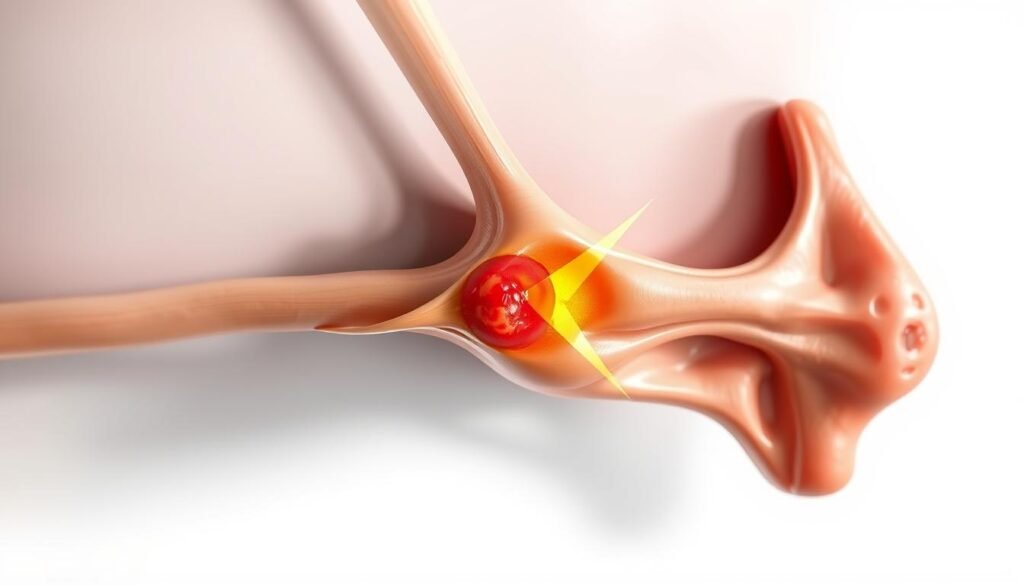
Occipital Neuralgia
Occipital neuralgia is characterized by paroxysmal shooting or stabbing pain in the distribution of the occipital nerves. This condition often presents with tenderness over the affected nerve and may be accompanied by diminished sensation or dysesthesia. Occipital nerve blocks can provide significant relief by interrupting the pain signals transmitted through these nerves.
The diagnostic value of these blocks also lies in their ability to confirm the involvement of occipital nerves in the pain mechanism, offering a temporary solution for patients.
Migraines
Migraines, while not directly caused by occipital nerve irritation, can benefit from occipital nerve blocks. The procedure interrupts pain signals that contribute to migraine pathophysiology, particularly in cases of chronic migraine. By blocking these signals, patients may experience a reduction in the frequency and severity of their migraines.
Studies have shown that occipital nerve blocks can be an effective treatment option for patients with refractory migraines, providing relief when other treatments have failed.
Cluster Headaches
Cluster headaches are known for their excruciating unilateral periorbital pain, occurring in cyclical patterns. Occipital nerve blocks may be used as part of a comprehensive treatment approach for cluster headaches, especially when conventional therapies have proven insufficient. The blocks can help alleviate the severe pain associated with these headaches.
The use of occipital nerve blocks in treating cluster headaches highlights their versatility in managing various headache disorders.
Cervicogenic Headaches
Cervicogenic headaches originate from structural issues in the cervical spine and associated soft tissues. These headaches often involve referred pain through the occipital nerves, making occipital nerve blocks an effective treatment option. By targeting the nerves involved, these blocks can provide significant pain relief.
| Headache Type | Characteristics | Response to Occipital Nerve Blocks |
|---|---|---|
| Occipital Neuralgia | Paroxysmal shooting pain, tenderness over affected nerve | Significant relief by interrupting pain signals |
| Migraines | Severe headache, often with aura, nausea, and sensitivity to light | Effective in reducing frequency and severity, especially in chronic cases |
| Cluster Headaches | Excruciating unilateral periorbital pain, cyclical patterns | Provides relief as part of a comprehensive treatment approach |
| Cervicogenic Headaches | Originates from cervical spine issues, referred pain through occipital nerves | Effective in providing pain relief by targeting involved nerves |

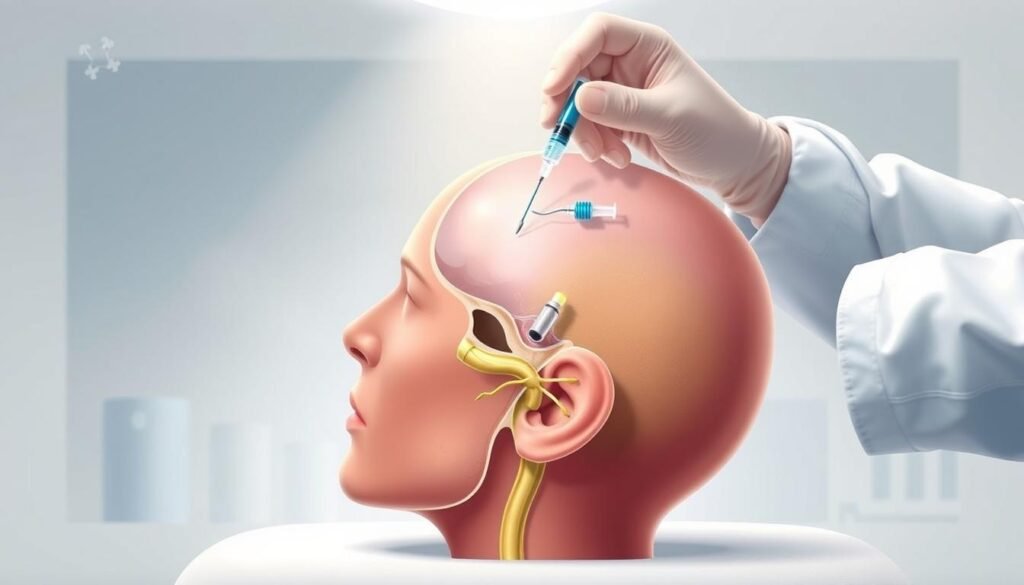
The Occipital Nerve Block Procedure

The procedure for an occipital nerve block involves several key steps that are crucial for its success. It’s typically performed as an outpatient procedure, meaning you can go home the same day.
Pre-Procedure Preparation
Before undergoing an occipital nerve block, patients undergo a thorough evaluation. This includes a review of their medical history, a physical examination, and a discussion of their current medications. It’s particularly important to disclose any blood thinners, as they may need to be temporarily discontinued before the procedure.
Landmark-Based Technique
The landmark-based technique is one method used to perform an occipital nerve block. This involves identifying specific anatomical landmarks, such as the occipital protuberance and mastoid process on the nuchal ridge. The GON (Greater Occipital Nerve) is typically located one-third of the distance from the occipital protuberance to the mastoid process, often just medial to the occipital artery. Due to anatomical variations, this approach may require larger volumes of local anesthetic (3-5 cc) to ensure successful blockade.
Ultrasound-Guided Technique
The ultrasound-guided technique represents a more precise advancement in performing nerve blocks. It allows for the visualization of the GON at the level of C2 as it courses between the obliquus capitis inferior and semispinalis capitis muscles. This enables more targeted administration of medication. The use of ultrasound guidance offers several advantages, including better visualization of the nerve, avoidance of nearby vascular structures, and potentially better outcomes for patients with proximal nerve entrapment.
The entire procedure usually lasts around 15 minutes. You’ll be awake during the procedure, but you’ll receive IV medicine to reduce anxiety and provide some pain relief. Your healthcare team will monitor your vital signs throughout the process.
Medications Used in Occipital Nerve Blocks
The medications used in occipital nerve blocks are key to their therapeutic effect. These blocks typically involve a combination of local anesthetics and steroid medications to provide both immediate and sustained pain relief.
Local Anesthetics
Local anesthetics, such as lidocaine (1-2%) and bupivacaine (0.25-0.5%), are used to provide immediate pain relief by blocking nerve signals. Lidocaine offers a rapid onset of action, while bupivacaine provides a longer duration of effect. The mechanism of action involves temporarily blocking sodium channels in nerve membranes, thereby interrupting pain signal transmission. The effect of the local anesthetic typically wears off within four hours.

Steroid Medications
Steroid medications, including betamethasone, dexamethasone, methylprednisolone, and triamcinolone, are used to reduce inflammation around the affected nerves, providing longer-term pain relief. These corticosteroids are often combined with local anesthetics to achieve both immediate and sustained relief. The steroid effect can take up to two weeks to become fully apparent, offering a prolonged therapeutic benefit beyond the initial anesthetic effect.
Benefits of Occipital Nerve Blocks
Occipital nerve blocks have emerged as a valuable treatment option for various headache disorders, offering both therapeutic and diagnostic benefits. These blocks are not only effective in providing pain relief but also serve as a diagnostic tool to help clinicians understand the underlying causes of headache disorders.
Pain Relief Benefits
One of the primary benefits of occipital nerve blocks is their ability to provide rapid pain relief for patients suffering from various headache disorders. Significant therapeutic benefits are observed often within minutes to hours following the procedure. The duration of pain relief varies considerably among patients, with some experiencing benefits lasting days to months. This can potentially reduce reliance on daily analgesic medications and improve overall quality of life.
- Rapid pain relief for headache disorders
- Variable duration of pain relief among patients
- Potential reduction in daily analgesic medication use
Diagnostic Benefits
Beyond pain relief, occipital nerve blocks serve as valuable diagnostic tools. They help clinicians differentiate between various headache disorders and identify the specific pain generators involved in a patient’s symptoms. A positive response to an occipital nerve block confirms the involvement of occipital nerves in the pain mechanism and guides subsequent treatment decisions.
| Diagnostic Use | Benefits |
|---|---|
| Differentiating headache disorders | Identifies specific pain generators |
| Confirming occipital nerve involvement | Guides subsequent treatment decisions |
Potential Risks and Side Effects
Occipital nerve blocks are considered a relatively safe procedure, but like any medical intervention, they come with potential risks and side effects. Understanding these risks is crucial for informed decision-making.
Common Side Effects
Common side effects following occipital nerve blocks are typically mild and transient. These may include pain at the injection site, temporary numbness or tingling in the scalp, dizziness, and mild headache. Such effects generally resolve within 24-48 hours without specific intervention. For more detailed information on the procedure and its effects, visit Healthline’s Occipital Nerve Block page.
| Side Effect | Duration |
|---|---|
| Pain at injection site | 24-48 hours |
| Numbness or tingling | Temporary |
| Dizziness | 24-48 hours |
Rare Complications
Although rare, serious complications can occur. These may include nerve damage, allergic reactions to the medications used, and inadvertent intravascular injection leading to systemic toxicity. Patients with diabetes should be monitored for potential changes in blood sugar levels due to the corticosteroid component of the injection.
| Complication | Description |
|---|---|
| Nerve damage | Prolonged sensory disturbances |
| Allergic reactions | Reaction to medications used |
| Systemic toxicity | Due to intravascular injection |
Recovery and Effectiveness
Understanding what to expect after an occipital nerve block is crucial for managing pain and assessing its effectiveness. The procedure is a treatment option for various headache disorders, including migraines and cluster headaches.
What to Expect After the Procedure
Immediately following an occipital nerve block, patients typically experience numbness in the distribution of the blocked nerves, confirming proper medication delivery. This numbness generally subsides within 4-6 hours as the local anesthetic effect diminishes. During the first 24-48 hours, patients may experience a temporary return or slight worsening of their baseline headache symptoms before the anti-inflammatory effects of the corticosteroid component begin to manifest.
For more information on preparing for a nerve block procedure, you can visit this resource to learn more about the process.
Duration of Pain Relief
The full therapeutic benefit of an occipital nerve block typically develops over 3-7 days as the corticosteroid reduces inflammation around the affected nerves, with the maximum effect often observed within 7-14 days post-procedure. The duration of pain relief varies significantly among patients, ranging from several days to several months. Factors influencing the longevity of the effect include the underlying diagnosis, chronicity of symptoms, presence of structural abnormalities, and individual response to corticosteroids.
Some patients experience significant but short-lived pain relief, and for them, repeat procedures may be considered. However, most practitioners recommend limiting steroid injections to 3-4 per year at minimum three-month intervals to minimize potential systemic effects of repeated corticosteroid administration.
Conclusion
In conclusion, occipital nerve blocks have emerged as a valuable treatment option for various headache disorders, offering both diagnostic clarity and therapeutic benefit for appropriately selected patients.
The procedure’s minimally invasive nature and relatively low risk profile make it an important consideration in the management of patients with refractory headaches, particularly those with occipital neuralgia, certain migraines, and cervicogenic headaches.
While not a permanent solution for most patients, occipital nerve blocks can provide substantial temporary relief, improve function and quality of life, and in some cases, interrupt the cycle of chronic pain. According to recent studies, the evolution of technique from landmark-based to ultrasound-guided approaches has enhanced precision and safety, potentially improving outcomes and reducing procedural complications.
Future directions in nerve block therapy include refinement of patient selection criteria, optimization of medication combinations and dosing, and development of sustained-release formulations. These advancements aim to maximize long-term benefit for patients suffering from chronic headache disorders.
Overall, occipital nerve blocks represent a significant advancement in the treatment and management of headache pain, providing a valuable therapeutic option for patients and healthcare providers alike.

