Chronic pelvic pain can be debilitating, affecting daily life and overall well-being. For those suffering from this condition, a pudendal nerve block offers a potential solution. This procedure involves an injection in the pelvic region to provide temporary pain relief.
The pudendal nerve plays a crucial role in pelvic sensation, and blocking its signals can significantly reduce discomfort. Healthcare providers use this nerve block for diagnostic and therapeutic purposes, helping patients manage their pain more effectively.
Understanding what to expect during a nerve block procedure can alleviate anxiety and prepare patients for the treatment. This article aims to provide a comprehensive overview, guiding you through the process and its benefits.
Key Takeaways
- A pudendal nerve block is used for managing chronic pelvic pain.
- The procedure involves an injection to block pain signals.
- It serves both diagnostic and therapeutic purposes.
- Understanding the procedure can help alleviate patient anxiety.
- This treatment offers temporary pain relief for various pelvic conditions.
Understanding Pudendal Nerve Block
A pudendal nerve block is a specialized procedure used for pain relief in the pelvic region. This technique involves an injection that targets the pudendal nerve.
Definition and Purpose
A pudendal nerve block is defined as a nerve block that provides anesthesia or pain relief by targeting the pudendal nerve. The dual purpose of this block is to serve as both a diagnostic tool and a therapeutic treatment.
When Is a Pudendal Nerve Block Recommended
Healthcare providers recommend a pudendal nerve block for patients suffering from chronic pelvic pain or for certain medical procedures requiring regional anesthesia. This nerve block is particularly useful in managing pain that is difficult to treat with other methods.
Diagnostic vs. Therapeutic Applications
Nerve blocks, including pudendal nerve blocks, are used diagnostically to identify the source of pain and therapeutically to provide relief. The block can offer both short-term and potentially longer-term pain relief for patients.
Anatomy of the Pudendal Nerve
Understanding the anatomy of the pudendal nerve is crucial for diagnosing and treating various pelvic floor disorders. The pudendal nerve is a complex nerve that provides both motor and sensory innervation, playing a vital role in controlling the pelvic floor muscles and providing sensory innervation to the perineum and external genitalia.
Location and Path of the Pudendal Nerve
The pudendal nerve originates from the S2-S4 sacral nerve roots, arising from the sacral plexus. It then passes through the greater sciatic foramen, piercing the sacrospinous and sacrotuberous ligaments, before reentering the pelvis through the lesser sciatic foramen. The nerve courses through the pudendal canal, also known as Alcock’s canal, which is formed by the fascia of the obturator internus muscle. This canal carries the neurovascular bundle, including the pudendal artery, vein, and nerve, before exiting medial to the ischial spine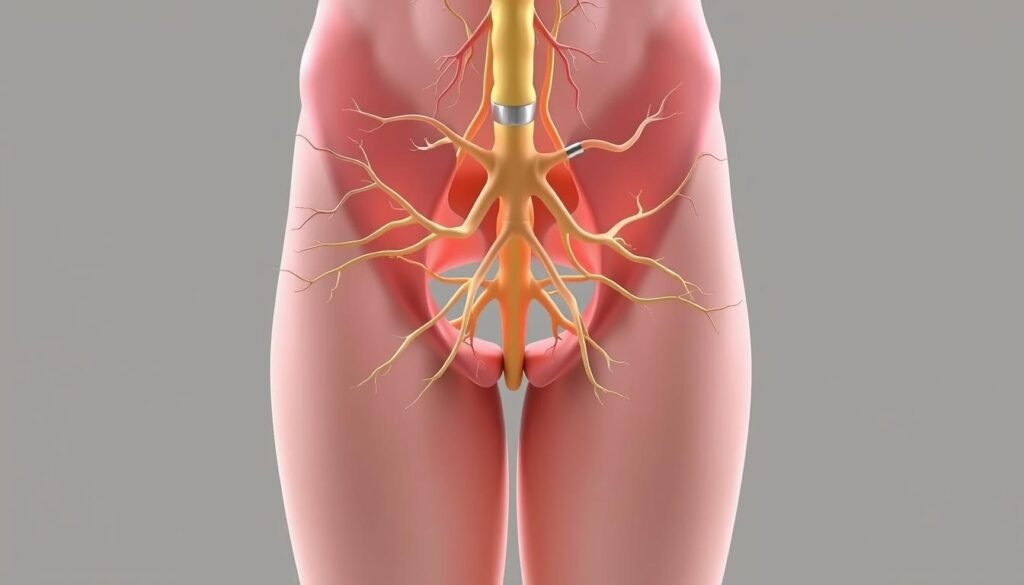
Areas Innervated by the Pudendal Nerve
The pudendal nerve provides sensory innervation to the rectal canal, anus, perineum, and external genitalia. It has three main branches: the dorsal nerve of the penis/clitoris, the perineal nerve, and the inferior rectal nerve. These branches innervate the external genitalia, perineum, and anal region, playing a crucial role in both sensory perception and motor function, particularly in controlling the pelvic floor muscles and sexual function.
Medical Conditions Treated with Pudendal Nerve Blocks

Pudendal nerve blocks have emerged as a crucial treatment option for various medical conditions characterized by chronic pain. These blocks are particularly effective for conditions that involve the pudendal nerve and its innervated areas.
Pudendal Neuralgia
Pudendal neuralgia is a neuropathic condition characterized by severe pain in the areas innervated by the pudendal nerve. Symptoms include burning, stabbing, or shooting pain in the genital region, perineum, and rectum, typically worsening when sitting.
Chronic Pelvic Pain
Chronic pelvic pain is another condition where pudendal nerve blocks are beneficial. This type of pain can be debilitating and is often resistant to conservative treatments. The blocks serve as both diagnostic and therapeutic interventions.
Use During Vaginal Delivery
Pudendal nerve blocks are also utilized during vaginal delivery to provide regional anesthesia during the second stage of labor and for episiotomy repair. This application helps manage pain effectively, making the process less traumatic for the mother.
Preparing for Your Pudendal Nerve Block
Understanding what to expect and how to prepare for your pudendal nerve block can significantly reduce anxiety and improve outcomes. As a patient undergoing this procedure, it’s crucial to follow your healthcare provider’s instructions carefully to ensure your safety and the effectiveness of the pudendal nerve block.
Pre-Procedure Instructions
Before the procedure, your healthcare provider will give you specific instructions, which may include adjusting your medications and fasting for a certain period. It’s essential to inform your provider about all medications, supplements, and allergies you have to minimize the risk of complications related to pain management.
What to Bring to Your Appointment
On the day of your pudendal nerve block, bring your insurance information, relevant medical records, and a list of your current medications. Arranging for someone to drive you home is also recommended, as driving is typically not advised after a nerve blocks care and time are important for a smooth recovery.

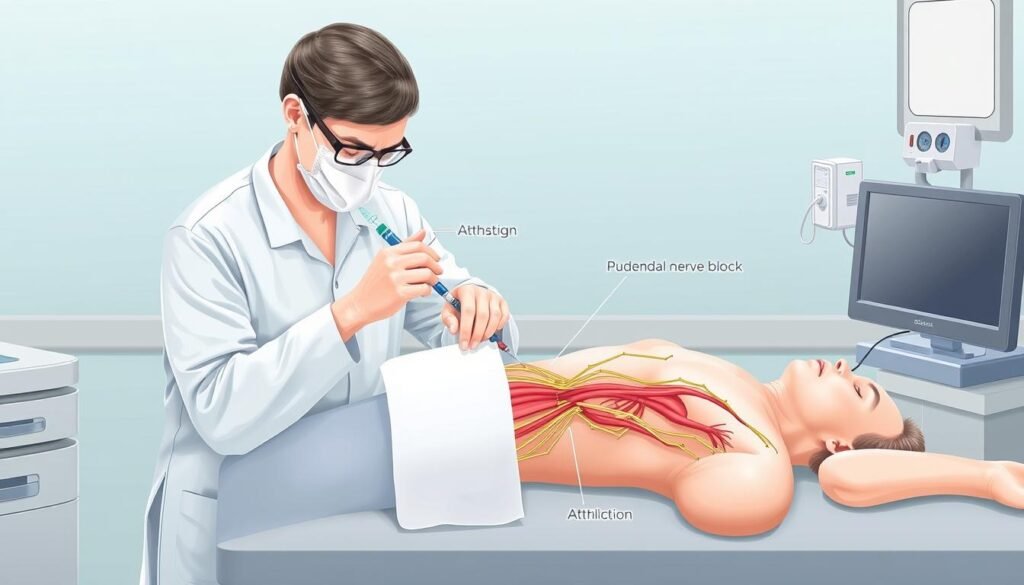
The Pudendal Nerve Block Procedure Step by Step
Understanding the step-by-step process of a pudendal nerve block can help alleviate patient concerns. The procedure involves several critical stages, from patient positioning to the injection of medication.
Patient Positioning and Preparation
The patient is positioned prone, and the skin is prepped in a standard sterile manner. This preparation is crucial for minimizing the risk of infection and ensuring a safe procedure.
Imaging Guidance Techniques
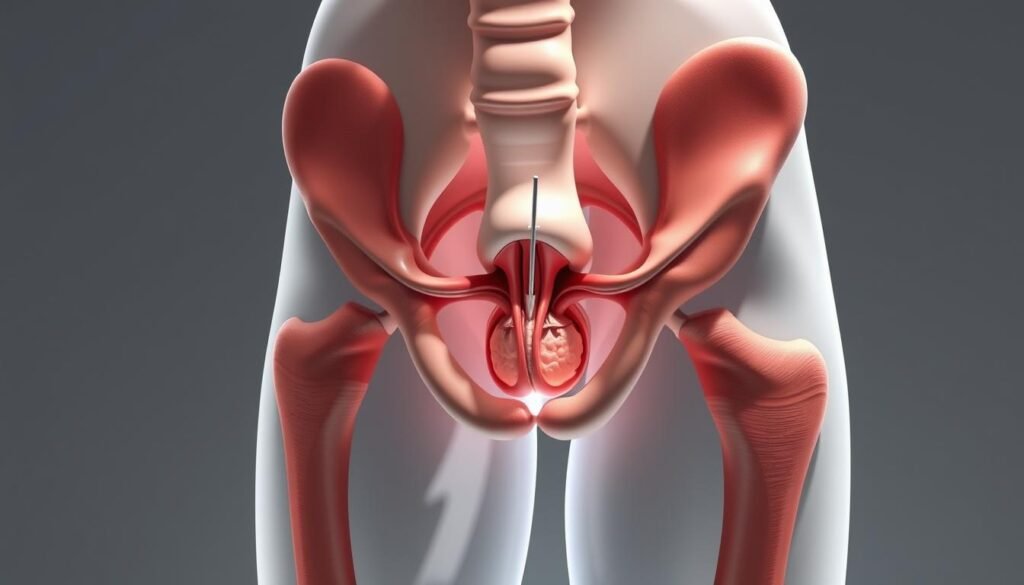 fluoroscope is used to provide an AP view of the pelvis, helping to identify the ischial spine. The fluoroscope is then rotated ipsilaterally until the ischial spine becomes prominent.
fluoroscope is used to provide an AP view of the pelvis, helping to identify the ischial spine. The fluoroscope is then rotated ipsilaterally until the ischial spine becomes prominent.
Needle Placement and Injection Process
Using fluoroscopic guidance, a sterile 22 gauge 5 inch spinal needle is advanced to the tip of the ischial spine. The needle is then used to administer local anesthetic, and potentially corticosteroids, to the target area around the pudendal nerve.
Duration of the Procedure
The procedure typically takes between 15-30 minutes. During this time, patients are monitored for any adverse reactions, and the effectiveness of the nerve block is assessed.
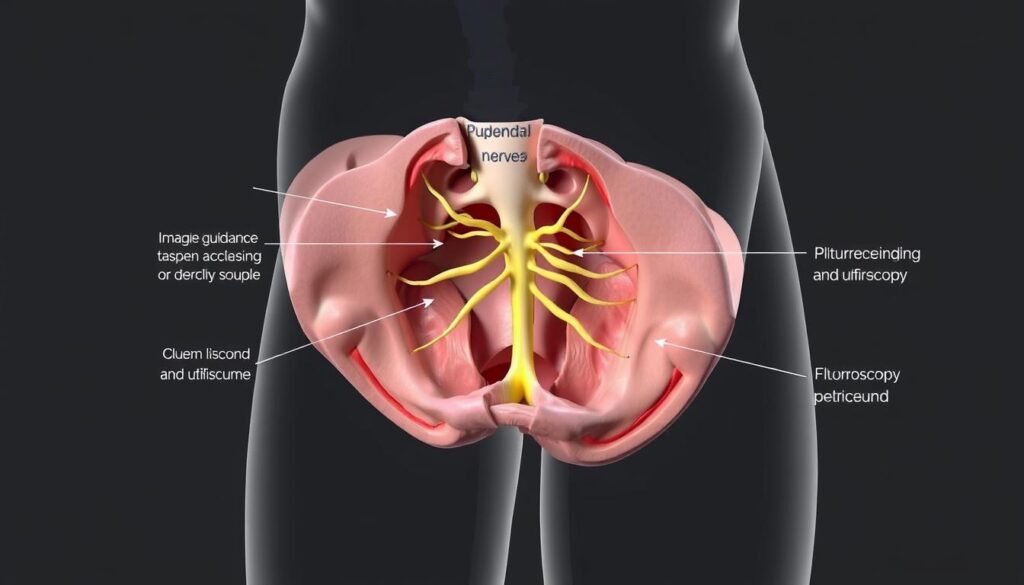
Types of Imaging Guidance for Pudendal Nerve Blocks
There are several imaging guidance techniques used for pudendal nerve blocks, each with its own advantages. The choice of imaging modality can significantly impact the success and safety of the procedure.
Fluoroscopic Guidance
Fluoroscopic guidance is a commonly used technique for pudendal nerve blocks. It involves using a fluoroscope to visualize the bony landmarks, particularly the ischial spine, to guide needle placement. A fluoroscopically guided technique typically employs a 5-15° ipsilateral oblique angulation of the pelvis, with the patient lying prone.
Ultrasound Guidance
Ultrasound guidance provides real-time visualization of soft tissues, blood vessels, and the pudendal nerve itself. This method can be particularly advantageous for certain patients, offering a safe and effective alternative to fluoroscopy. Studies have shown that while the degree of neural blockade is similar between ultrasound and fluoroscopic guidance, the time to complete the procedure under ultrasound can be significantly longer.
CT-Guided Procedures
CT-guided procedures offer precise three-dimensional imaging, making them ideal for complex cases or when other guidance methods are challenging. This technique allows for accurate needle placement and can be particularly useful in patients with anatomical variations.
| Imaging Technique | Advantages | Limitations |
|---|---|---|
| Fluoroscopic Guidance | Visualizes bony landmarks | Radiation exposure |
| Ultrasound Guidance | Real-time soft tissue visualization | Operator-dependent |
| CT-Guided Procedures | Precise 3D imaging | Higher radiation dose |
Medications Used in Pudendal Nerve Blocks
To achieve optimal results, pudendal nerve blocks utilize a range of medications with distinct mechanisms of action. The selection of these medications is critical for effective pain management.
Local Anesthetics
Local anesthetics such as lidocaine and bupivacaine are commonly used in pudendal nerve blocks. They work by temporarily blocking nerve signals, providing immediate pain relief. The choice between different local anesthetics depends on the desired duration of action and patient-specific factors.
Corticosteroids
Corticosteroids, like triamcinolone, are used to reduce inflammation around the pudendal nerve. By decreasing inflammation, corticosteroids can provide longer-lasting pain relief. The use of corticosteroids is particularly beneficial for patients with inflammatory components to their pain.
Medication Combinations
A combination of medications is often used to achieve both immediate and long-term pain relief. For example, a solution of 2 mL of 2% lidocaine mixed with 2 mL of 0.25% bupivacaine, and 1 mL of triamcinolone solution (40 mg/mL) can be used as the injectate for pudendal nerve blocks. This combination leverages the benefits of both local anesthetics and corticosteroids.
| Medication Type | Example | Primary Use |
|---|---|---|
| Local Anesthetics | Lidocaine, Bupivacaine | Immediate pain relief |
| Corticosteroids | Triamcinolone | Long-term pain relief through inflammation reduction |
| Combination | Lidocaine + Bupivacaine + Triamcinolone | Both immediate and long-term pain relief |
Potential Risks and Complications
Understanding the potential risks and complications of pudendal nerve blocks is crucial for informed decision-making. While generally considered safe, like any medical procedure, there are associated risks.
Common Side Effects
Common side effects of pudendal nerve blocks include temporary numbness, bruising at the injection site, and a temporary increase in pain. These effects are typically short-lived and resolve on their own.
Rare but Serious Complications
Rare but serious complications can occur, including infection, nerve damage, bleeding, and adverse reactions to the medications used in the block. Inadvertent blockade of nearby structures can lead to temporary bladder or sphincter dysfunction.
| Complication | Description |
|---|---|
| Infection | Rare, but can occur at the injection site |
| Nerve Damage | Temporary or permanent damage to the pudendal nerve |
| Bleeding | Minor bleeding or hematoma at the injection site |
When to Seek Medical Attention
Patients should seek immediate medical attention if they experience signs of infection, severe pain, or neurological symptoms after a pudendal nerve block. Monitoring for these complications is crucial in the recovery period.
Recovery After a Pudendal Nerve Block
The recovery period following a pudendal nerve block is a critical time for patients to monitor their symptoms and pain levels. This phase is essential for assessing the effectiveness of the procedure.
Immediate Post-Procedure Care
After the pudendal nerve block procedure, patients are monitored in a recovery area. Here, healthcare professionals observe the initial effects of the local anesthetic and ensure there are no immediate complications. Patients are then discharged with instructions to monitor their pain levels and symptoms closely.
Activity Restrictions
Patients are advised to resume activities gradually. A pelvic rehabilitation program is recommended, focusing on strengthening gluteal, hamstring, and pelvic floor muscles. This helps in achieving optimal pain relief. Patients should avoid strenuous activities for a few days post-procedure.
When to Expect Results
The pudendal nerve block provides immediate relief due to the local anesthetic, while the corticosteroids take a few days to exhibit their anti-inflammatory effects. Patients are instructed to keep track of their pain levels and schedule a follow-up appointment approximately four weeks later to assess the procedure’s effectiveness.
Follow-Up Care and Additional Treatments
Follow-up care after a pudendal nerve block is essential for evaluating pain relief and guiding further treatment. This care involves scheduled appointments with healthcare providers to assess the procedure’s effectiveness.
Monitoring Your Response
Healthcare providers closely monitor a patient’s response to the pudendal nerve block. If a patient reports at least 50% pain relief, a second confirmatory block may be considered to confirm the pudendal nerve as the pain source.
Repeat Procedures
Some patients may benefit from a series of pudendal nerve blocks to achieve optimal pain relief. The decision to proceed with repeat procedures is based on the patient’s response to the initial block.
Alternative and Complementary Treatments
In addition to pudendal nerve blocks, patients may be advised to resume a pelvic rehabilitation program. This program focuses on strengthening the gluteal, hamstring, and pelvic floor muscles.
| Treatment Option | Description | Benefits |
|---|---|---|
| Pudendal Nerve Blocks | Injection of medication to block pain | Pain relief, diagnostic tool |
| Pelvic Rehabilitation | Physical therapy to strengthen pelvic muscles | Improved muscle strength, pain management |
| Pulsed Radiofrequency Ablation | Procedure to disrupt pain signals | Long-term pain relief |
Conclusion
For individuals experiencing persistent pelvic pain, pudendal nerve blocks provide a promising avenue for both diagnosis and treatment. The procedure involves injecting a local anesthetic near the pudendal nerve to block pain signals, offering relief to patients suffering from chronic pelvic pain and pudendal neuralgia. When performed by experienced providers using proper imaging guidance, pudendal nerve blocks are generally safe and can be an effective part of a comprehensive treatment plan. It’s essential for patients to have realistic expectations and understand that this procedure is often used in conjunction with other therapies. By doing so, patients can make informed decisions about their care and potentially achieve significant pain relief.

