When pain steals time with family, work, or a walk in the park, hope matters. I know how heavy that worry feels when standing and walking become chores instead of joys.
If you’re exploring a treatment option called the Superion Indirect Decompression System, this concise guide explains what it offers for lumbar spinal stenosis and everyday relief.
This minimally invasive implant sits between spinous processes to open space around compressed nerves. The procedure is often a same-day outpatient visit through a small incision, preserving spine motion and offering a reversible alternative to open surgery.
Backed by FDA approval and multi-year outcomes, many patients report significant pain improvement and faster recovery. For clinical data and longer-term results, see this summary on patient outcomes at the National Library of Medicine: clinical outcomes and follow-up.
Key Takeaways
- Minimally invasive option for lumbar spinal stenosis that preserves motion.
- Same-day outpatient procedure with small incisions and short recovery time.
- Proven safety and multi-year effectiveness supported by FDA approval.
- Designed to reduce pain when standing and walking without removing bone.
- Good choice for patients seeking an alternative to open surgery after other treatments fail.
Who Benefits from Minimally Invasive Relief for Lumbar Spinal Stenosis
Many people with lower back narrowing find daily walking becomes painful and limiting. Moderate lumbar changes often show up on MRI or CT and match the symptoms below.
https://www.youtube.com/watch?v=fpBS5Gosa40
Common signs of moderate lumbar spinal stenosis
Leg pain, numbness, or cramping that worsens with standing or walking and eases with sitting is a hallmark sign. This pattern suggests the nerves in the lower back are compressed.
If you lean forward (for example, over a shopping cart) and feel relief, that posture clue points toward nerve compression that may improve when space is restored.
When conservative and interventional therapies haven’t provided adequate pain relief
Many patients try physical therapy, medications, and injections first. If these conservative interventional therapies fail to provide adequate pain relief, the procedure often recommended focuses on restoring room for the nerves so you can stand and walk more comfortably.
Your care team will confirm candidacy after updated MRI or CT plus lumbar X‑rays with flexion‑extension views. If there is concern for bone loss, a DEXA scan may be added.
- If you’ve experienced adequate pain despite non‑surgical care for at least six months, discuss options with your doctor.
- Schedule an appointment to review imaging and next steps toward predictable relief.
Superion Indirect Decompression System
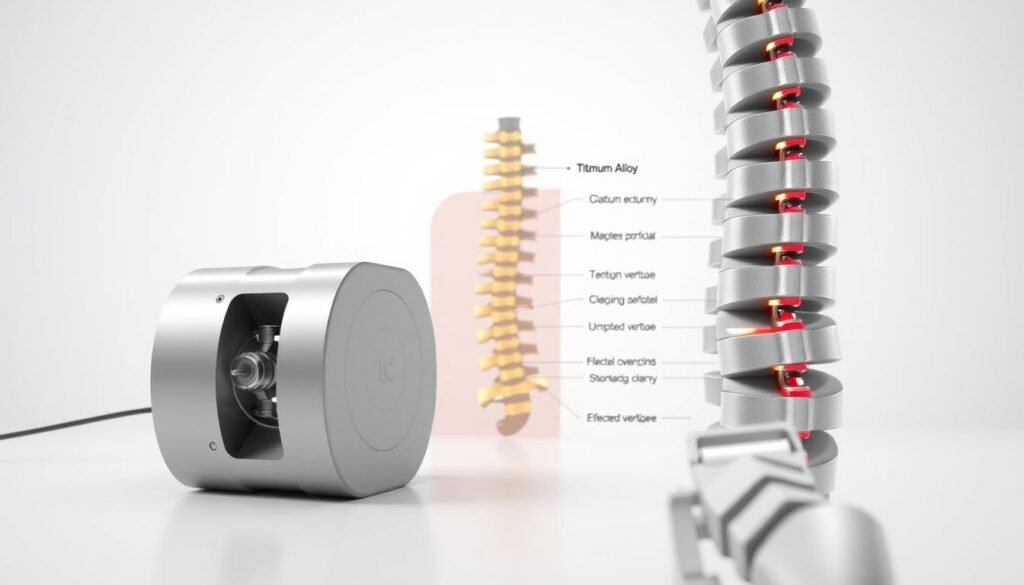
This titanium spacer offers a focused way to ease pressure on the lower spine while keeping motion intact.
The device sits between spinous processes and acts as an extension blocker. It creates the same opening you feel when leaning forward, so irritated nerves get relief without removing bone.
How it works as an extension blocker
By limiting painful backward bending, the implant decreases pinching at the treated level. That lift reduces pressure on nerves and can ease leg and lumbar pain.
Minimally invasive outpatient procedure
The procedure is outpatient and often completed one hour or less per level. Surgeons use fluoroscopic imaging and a small incision to place the titanium device. Anesthesia may be general or sedation for comfort.
Implant features and safety
The implant unique comes in multiple sizes so it can accommodate patient spine anatomy. These sizes accommodate patient needs for a precise fit and help protect nerves around spine structures.
Effectiveness and setting
FDA‑approved with outcomes to 60 months, this decompression system offers a predictable treatment option for selected lumbar cases. Talk with your surgeon about candidacy and expected recovery.
What to Expect: From Candidacy Evaluation to Lasting Relief
A clear plan starts with imaging and a conversation about what relief looks like for you. Your path begins with a consultation to confirm lumbar spinal stenosis and align treatment goals. Expect updated MRI or CT and flexion‑extension X‑rays to check motion at the affected level.

Preoperative steps
If bone health is a concern, a DEXA scan helps tailor care and reduce risk. Your team reviews medications, prior interventional therapies, and the timeline for appointments before the procedure.
The procedure timeline
On procedure day, the team uses fluoroscopic guidance and a small incision — about 1 cm to 1 inch — to place the device. The outpatient procedure is typically completed one hour per level or less, so most people go home the same day.
Preserving motion and anatomy
This approach preserves spinal motion and native anatomy while reducing the forward‑extension pinching that causes pain when standing or walking. Tissue disruption is minimal, which often means faster recovery than open surgery.
- Your care plan starts with accurate imaging and targeted evaluation.
- Procedure simple perform completed through a tiny incision with fluoroscopy.
- Most patients notice gradual pain reduction and improved walking over weeks to months.
- If interventional therapies least six months have not helped, discuss this option with your surgeon and schedule an appointment for evaluation.
Conclusion
If non‑surgical treatments fall short, a minimally invasive implant can restore space around irritated nerves with less downtime. This option — described as superion indirect decompression — aims to ease leg and back pain while keeping motion intact.
The indirect decompression system uses sized implants so the sizes accommodate patient spine anatomy and protect nearby nerves. It supports moderate lumbar cases of lumbar spinal stenosis without removing bone, offering a shorter recovery than open surgery.
Candidates typically try conservative interventional therapies for at least six months before considering the procedure. If you’ve experienced inadequate pain relief, schedule an appointment to review imaging and next steps.
Talk with your surgeon to learn if this treatment option called superion indirect is the right bridge between therapy and major surgery and to plan care that fits your goals and activity level.

