I remember the day a friend told me a small implant changed their life—sudden hope after years with relentless pain.
Today, nearly 50 million people in the United States live with chronic pain. Neurostimulation devices deliver low-voltage pulses to the spinal cord or peripheral targets to interrupt pain signals before they reach the brain.
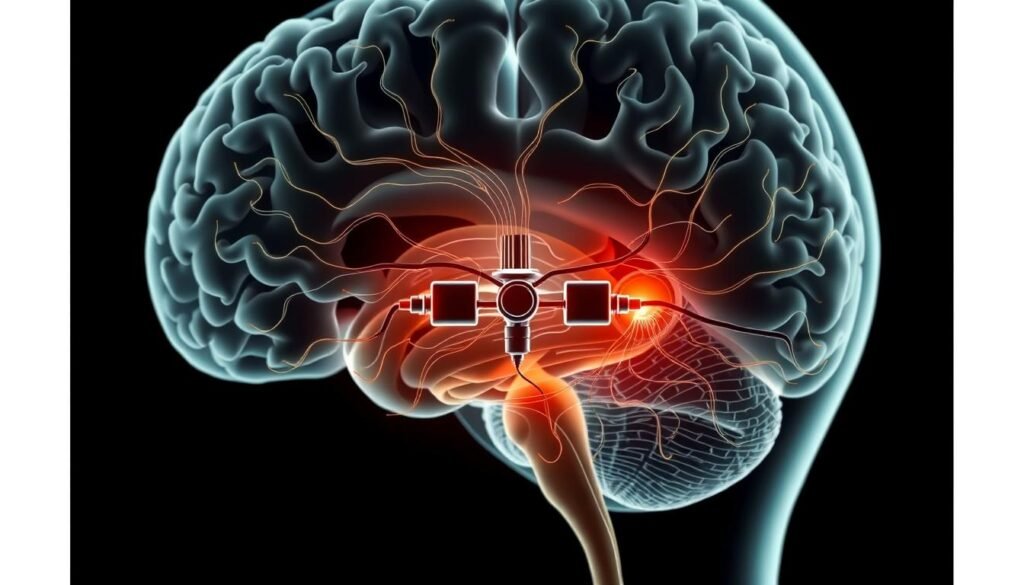
This guide lays out the full landscape: how these systems work, core components like the neurostimulator, leads, and programmer, and the main families—spinal cord, dorsal root ganglion, peripheral, sacral, vagus, and deep brain stimulation.
With decades of data and FDA-cleared systems from Abbott, Medtronic, and Boston Scientific, modern neurostimulation offers reversible, customizable relief for many patients.
Use this overview as a starting point for informed talks with your care team about candidacy, trials, side effects, and treatment options that fit your goals.
Key Takeaways
- Neurostimulation devices modulate pain pathways to offer targeted relief and improved function.
- Core parts include an implantable or external device, insulated leads, and a programmer.
- Several families address different pain conditions—choice depends on pain location and patient needs.
- Decades of clinical use and brands like Abbott and Medtronic support safety and effectiveness.
- Talk with a pain specialist about trials, follow-up care, costs, and realistic expectations.
What nerve stimulators are and how they relieve chronic pain today
Targeted pulses change how the body senses persistent pain.
Neurostimulation uses controlled electrical impulses to alter how pain signals travel between the spinal cord and the brain. These devices reduce the intensity of chronic pain by interrupting or modulating key pathways rather than destroying tissue.
How it works: low-voltage electrical pulses are delivered near nerves or within the epidural space to block or change the signal before the brain registers it. This modulation can let people move and sleep with less reliance on systemic medications.
Modern systems have three core parts: a neurostimulator (the generator and power source), thin insulated leads placed near the cord or target nerve, and a handheld programmer clinicians and patients use to fine-tune settings.
Many devices are fully implantable; others are external and radio‑frequency powered. Trials let patients test real‑world relief before a longer implant. With decades of clinical use and ongoing innovation, neurostimulation remains an adjustable, reversible treatment worth discussing with a specialist.
Implanted vs. external neurostimulation devices: key differences and use cases
Deciding between an implanted system and an external option depends on expected symptom duration, medical risk, and daily goals.
When to consider long-term implanted systems
Implanted devices place leads near target nerves or in the epidural space with a small generator under the skin. This design delivers ongoing, programmable stimulation for predictable, day-to-day relief.
Long-term implants suit patients with persistent chronic pain after conservative care who need steady pain management to preserve function and activity.
Where external, noninvasive options fit for short-term relief
External systems sit on the skin and deliver electrical energy through surface electrodes. They are easy to start and stop and often used for intermittent flares or when surgery is not appropriate.
These radio‑frequency powered neurostimulation devices also help test target coverage during diagnostic trials before committing to an implant.
- Shared strength: Both device classes are programmable by clinicians and often adjustable by patients within safe ranges.
- Selection factors: expected duration, lifestyle needs, medical risk, insurance, and follow‑up requirements.
- Integration: Both work best as part of a broader pain management plan alongside therapy, behavioral care, and medications.
| Feature | Implanted system | External system |
|---|---|---|
| Typical use | Sustained daily therapy for chronic conditions | Short-term control, trials, or intermittent flares |
| Placement | Leads near target or epidural + under‑skin generator | Surface electrodes or RF patch worn on skin |
| User control | Handheld programmer adjusts strength and location | Simple on/off and intensity controls; clinician-set limits |
| Best for | Persistent pain needing predictable relief | Diagnostic trials, comorbidity-limited patients, episodic pain |
Spinal cord stimulation for back pain and neuropathic pain
For many with chronic back and neuropathic pain, targeted cord therapy offers a reversible, programmable path to relief.
How it works: thin leads are placed in the epidural space so low-voltage electrical fields modulate dorsal column pathways. This cord stimulation changes how the spinal cord sends pain signals to the brain and can reduce the perception of pain.
Common indications and patient use
SCS is used when nonsurgical options fail. Typical candidates include people with persistent back pain after surgery, complex regional pain syndrome, amputation pain, and other neuropathic conditions such as painful diabetic neuropathy.
Modern devices have a generator under the skin and let patients turn therapy on and off and switch programs using a remote. That control helps match stimulation to daily needs.
Protocol advances and outcomes
High-frequency and novel waveform protocols often improve coverage and comfort, sometimes without paresthesias. New FDA-cleared indications — for example Nevro’s Senza system for painful diabetic neuropathy — reflect ongoing innovation.
- Procedure flow: a minimally invasive trial tests real-world relief before permanent implant.
- Benefits: reduced pain intensity, better mobility, and lower reliance on systemic meds.
- Risks: infection, lead migration, or hardware issues; careful technique and follow-up reduce complications.
The SCS market is growing rapidly, driven by demand for drug-sparing treatments and improved technology. For a clear overview of patient experiences with neurostimulation devices, see this patient-centered review.
Dorsal root ganglion stimulation for focal, regional pain
Dorsal root ganglion (DRG) stimulation offers a focused option when pain maps to a small, specific area.
Dorsal root ganglion stimulation concentrates therapy at the sensory cell bodies that exit the spinal canal. This targeting enables highly specific coverage of painful dermatomes that standard spinal approaches can miss.
Targeting specific dermatomes in complex regional pain syndrome
Who benefits: patients with well‑mapped, localized chronic pain—for example CRPS affecting the foot, knee, groin, or hand—often see better outcomes with DRG than with broad-field stimulation.
Implantation usually involves percutaneous placement of leads next to the target DRG and a small implanted generator. Clinicians then program tailored settings during and after a trial period to tune coverage and comfort.
- DRG helps reduce touch‑evoked pain and hypersensitivity in confined areas.
- It can improve limb use and daily function with fewer off‑target sensations.
- Risks mirror other implants—infection and lead migration—so experienced teams emphasize precise placement and follow‑up.
When conservative care and broader field therapies underperform, DRG is a recognized next step before considering more central targets like deep brain stimulation. Ask your care team whether this targeted form of neurostimulation might fit your treatment plan for specific pain conditions.
Peripheral nerve stimulation and peripheral field stimulation
Targeted leads placed near named nerves or just under the skin can change how localized pain is felt.
Peripheral nerve stimulation targets specific named nerves, such as occipital or inguinal nerves, by placing small leads close to the nerve to reduce localized pain. Clinicians use this when pain maps to a clear spot and spinal solutions miss the target.
Peripheral field stimulation uses subcutaneous leads to create a wider pain‑relieving field over an area like the lower back or abdomen. This approach treats superficial pain that covers a region rather than a single nerve.
Common uses and combined strategies
- Occipital and supraorbital stimulation for chronic migraines and head pain.
- Inguinal stimulation for post‑hernia repair neuralgia.
- Clinic procedures such as the Reed (occipital + supraorbital) give broader head coverage.
- Combined programs (the Vega approach) layer spinal cord and peripheral methods to boost outcomes for select patients.
Typical care begins with mapping the painful area, a brief trial to test coverage, and a minimally invasive implant if effective. Day‑to‑day benefits include on‑demand adjustments and often fewer headache days or improved activity tolerance.
Risks include localized infection, lead migration, and skin irritation; secure anchoring and follow‑up lower these problems. Work with headache specialists and pain teams to match targets to triggers and lifestyle goals.
| Feature | Peripheral nerve stimulation | Peripheral field stimulation / Combined |
|---|---|---|
| Target | Single named nerve (occipital, inguinal) | Subcutaneous field; combined with SCS for layered coverage |
| Best for | Focal chronic pain and targeted neuropathic pain | Regional superficial pain such as lower back or abdominal areas |
| Typical benefit | Precise relief, fewer off‑target sensations | Broader coverage, complements spinal strategies for better overall relief |
Sacral nerve stimulation for pelvic floor and bladder dysfunction
Electrical pulses aimed at sacral roots can restore more normal pelvic floor function for many people.
What it does: Sacral nerve stimulation modulates sacral roots to normalize signals that control the bladder, bowel, and pelvic floor. An electrode sits near a sacral root and a small implanted generator delivers adjustable therapy.
Primary U.S. indications include refractory urinary urgency‑frequency, urinary and anal incontinence, and retention. Some patients with urgency or frequency also report reduced chronic pelvic pain after successful therapy.
Benefits reach beyond symptom counts: fewer urgent trips, better continence, and improved confidence at work and social events. Studies support durable response when responders are identified with a proper trial.
Patient selection and practical notes
- Consider when medication and behavioral therapy fail and quality of life is affected.
- Programming can be refined in clinic or with a patient remote to match daily patterns.
- Risks include infection and lead movement; careful placement and follow‑up lower these risks.
- Use alongside pelvic floor physical therapy and behavioral strategies for best outcomes.
| Feature | What to expect | Why it matters |
|---|---|---|
| Placement | Electrode by sacral root + under‑skin generator | Targeted modulation of bladder and bowel control |
| Primary uses | Urgency, incontinence, retention, some pelvic pain | Reduces daily bother and improves function |
| Follow‑up | Noninvasive programming, trials, periodic checks | Maintains durable relief and optimizes management |
Vagus nerve stimulation: implanted and noninvasive options
Vagus nerve stimulation taps a long cranial pathway to influence pain, mood, and internal organ signals.
Vagus nerve stimulation modulates the vagus nerve that links the brainstem to chest and abdominal organs. That wide reach can alter pain, mood, and autonomic balance and make it a useful tool in select conditions.
Conventional implanted VNS in the United States
Implanted VNS uses a small generator placed in the chest and leads to the cervical vagus. It is FDA‑cleared for drug‑resistant epilepsy and treatment‑resistant major depression.
Implanted therapy requires surgery, programming, and regular follow‑up. Clinicians may explore research protocols for movement disorders and chronic pain in select cases.
Noninvasive options for headache and migraine
Handheld, noninvasive devices apply short pulses to the neck for on‑demand stimulation. They are approved for episodic cluster headache and migraine in many regions.
- Advantages: no incision, favorable tolerability, and quick use during an attack.
- Integration: devices work best combined with medication and behavioral strategies.
- Experience: clinicians train patients and track symptom patterns to optimize timing and dosing.
Market growth reflects rising interest in noninvasive neurostimulation and drug‑sparing approaches. Expect coordination between neurology, psychiatry, and pain teams to choose the right pathway and set realistic goals for fewer attacks and improved daily function.
Deep brain stimulation for pain and movement disorders
Deep brain stimulation (DBS) places tiny electrodes inside specific brain regions to change how circuits handle pain and movement.
When DBS is considered: clinicians reserve this brain‑targeted treatment for patients who did not gain adequate relief from less invasive options such as spinal cord or dorsal root ganglion therapy. Typical candidates include people with central post‑stroke pain, atypical facial pain, and brachial plexus injury.
Key targets and rationale
Surgeons aim at precise nuclei to shape different aspects of pain.
- Thalamus (VPL/VPM) — modulates sensory transmission and intensity.
- PVG/PAG — activates descending pain inhibition pathways.
- Rostral ACC — addresses the emotional and affective dimension of pain.
What patients can expect
DBS for pain follows a staged pathway: multidisciplinary evaluation, imaging and target planning, implant surgery, then iterative programming over several visits. Outcomes include reduced pain intensity, better tolerance to touch or movement, and improved daily function for carefully selected patients.
| Feature | Indication | Target | Notes |
|---|---|---|---|
| Central post‑stroke pain | Severe central neuropathic pain | VPL/VPM or PAG | Considered after SCS/DRG failure; needs center expertise |
| Atypical facial pain | Refractory facial neuropathic pain | Thalamus (VPM) | Careful mapping and trial stimulation recommended |
| Movement disorders | Parkinson’s disease, tremor | Subthalamic nucleus / GPi | Well‑established use; drives market growth in DBS devices |
| General notes | Benefits vs risks | Rostral ACC for affective pain | Risks include bleeding, infection, and lead misplacement; long‑term follow‑up required |
Market and research: DBS is a mature treatment for movement disorders and a growing field for chronic pain. The global DBS devices market expanded from about USD 1.31 billion in 2021 and is projected to grow as indications and technologies evolve.
Patients should seek care at experienced centers and consider clinical trials when appropriate to access advanced protocols and careful long‑term follow‑up.
Types of nerve stimulators
Choosing the right stimulation approach starts with matching where and how pain is felt to what each device can cover.
Matching device categories to pain conditions and treatment goals
Major categories include spinal cord stimulation (SCS) for widespread neuropathic back and limb pain, dorsal root ganglion (DRG) for focal regional pain in defined dermatomes, peripheral nerve and field approaches for localized or subcutaneous pain, sacral stimulation for pelvic and bladder dysfunction, vagus stimulation (implanted or noninvasive) for select headache and seizure or mood indications, and deep brain stimulation (DBS) as a reserved option for complex central pain.
- SCS — broad coverage for chronic pain across limbs and trunk.
- DRG — targeted relief for well‑mapped regional symptoms.
- PNS/PFS — focal relief where a named nerve or field is the source.
- Sacral/VNS/DBS — specialized roles tied to organ function, headaches, or refractory central syndromes.
“Trials and programming flexibility are the keys to confident long‑term outcomes.”
Selection depends on size and depth of the painful area, triggers, comorbidities, lifestyle, MRI needs, and tolerance for follow‑up. Trials confirm responders, and programming options (battery life, rechargeability, paresthesia vs paresthesia‑free modes) let clinicians tailor therapy. Combining approaches, such as SCS with peripheral leads, can improve coverage in complex cases.
| Category | Best fit | Key patient considerations |
|---|---|---|
| Spinal cord stimulation | Widespread neuropathic back/limb pain | Desire predictable daily relief; check MRI compatibility |
| Dorsal root ganglion | Focal regional pain in dermatomes | Precise targeting needed; high programming specificity |
| Peripheral nerve / field | Localized or superficial pain | Less invasive; good for episodic or focal problems |
| Sacral / Vagus / DBS | Pelvic dysfunction, headaches/epilepsy, refractory central pain | Specialist centers; higher invasiveness for DBS |
Shared decision‑making with a multidisciplinary team helps align treatment options with patient goals and daily routines, improving the chance of meaningful relief and lasting benefit.
Candidates, evaluation, and trial procedures
When conservative approaches fall short, clinicians evaluate candidacy for targeted electrical therapy to restore function and reduce medication needs.
Who benefits: Ideal candidates are patients with persistent chronic pain despite medications, injections, and structured physical therapy. They want drug-sparing treatment options and improved daily function rather than total symptom elimination.
Evaluation is multidisciplinary. Teams gather medical history, imaging when needed, and perform psychological screening. Pain mapping helps match targets and clarify realistic goals for quality life gains.
Outpatient trials and programming
Outpatient trials place temporary leads to test coverage during normal activities over several days. Clinicians program settings and adjust stimulation to optimize comfort and effectiveness.
Success metrics focus on meaningful pain reduction, better sleep, more activity, and measurable quality life improvements. Those who respond in trials usually report higher long-term satisfaction after implant.
- External, noninvasive devices can be tried first when surgery isn’t suitable.
- Expect ongoing follow-up, occasional reprogramming, and patient training to use controllers effectively.
Shared decision-making ties selection and follow-up to rehabilitation and lifestyle goals. Open discussion about commitments and realistic outcomes helps patients choose the best treatment path.
Benefits, risks, and side effects to weigh
Understanding likely gains and possible complications helps patients choose a path that fits their goals.
Pain relief, reduced medication use, and improved function
Many people see meaningful pain relief after neurostimulation. That can mean better sleep, improved mobility, and more ability to work or exercise.
Some patients cut back on systemic pain medicines, which may lower drug side effects and interactions. Overall, responders often report higher quality life and greater independence.
Potential complications: infection, bleeding, nerve injury, device issues
Surgical risks include infection and bleeding. Most teams limit these with sterile technique and careful follow-up.
Neurologic events such as nerve irritation or injury are uncommon with experienced clinicians. When they occur, early evaluation reduces lasting harm.
Device-specific problems can include lead migration, hardware discomfort, or battery failure that may need reprogramming or revision. External systems can cause local skin irritation at electrode sites.
“A short pre-implant trial helps confirm likely benefit before accepting implant risks.”
- Summarizes benefit: substantial relief, better function, and improved quality life.
- Summarizes risk: infection, bleeding, neurologic injury, and device or skin side effects.
- Action points: informed consent, clear recovery timelines, and prompt access to support.
| Area | Expected benefit | What to watch for |
|---|---|---|
| Symptom control | Reduced pain and fewer flares | Need for reprogramming or revisions |
| Medication use | Lower opioid/analgesic doses | Monitor withdrawals and adjustments |
| Safety | Improved daily function | Infection, bleeding, nerve irritation |
Long-term management includes regular programming visits and early problem reporting to keep outcomes durable and safe.
Integrating neurostimulation with comprehensive pain management
When stimulation reduces pain signals, it creates a chance to rebuild strength and daily routines.
Neurostimulation is one pillar in a broader plan for chronic pain. It works best alongside physical therapy that restores movement patterns and strength safely.
Cognitive behavioral strategies and mindfulness help patients reduce distress, improve sleep, and pace activity. Targeted medications for neuropathic pain can complement stimulation and often let clinicians lower drug doses.
Coordinated care among pain physicians, therapists, and mental health professionals prevents fragmented treatment. Routine outcome tracking—pain scores, function scales, and sleep quality—guides programming tweaks and rehab progress.

Practical steps for lasting gains
- Start with a shared goal: reduce pain and restore activity.
- Use graded activity and conditioning as pain improves to reinforce function.
- Teach device use, flare planning, and healthy routines to maintain momentum.
- Address lifestyle factors—nutrition, weight, and smoking—to support outcomes.
“Treat the whole person, not just the pain generator.”
For deeper clinical context, see this systematic review and a patient-centered review that summarize multimodal approaches to neurostimulation and pain relief.
Devices, brands, and market outlook in the United States
Industry competition and new clearances are widening options for people with chronic pain.
Leading manufacturers
The U.S. market blends large medtech firms with focused innovators. Medtronic, Abbott, and Boston Scientific dominate clinical use and training programs.
Specialized players such as Nevro, electroCore, Aleva Neurotherapeutics, and EndoStim bring novel approaches and niche approvals that expand patient choice.
Growth trends and regulatory momentum
Markets for spinal cord, vagus, and deep brain stimulation are growing fast. The SCS segment may reach about USD 3.72B by 2027 (CAGR ~8.7%).
VNS is projected near USD 717.17M and DBS around USD 2.37B by 2027. Overall, the neurostimulation devices market could top USD 11.34B by 2027 (CAGR ~11.8%).
Recent milestones: FDA clearance for Nevro Senza in painful diabetic neuropathy and Breakthrough Device designation for the Unity HA Pulsante SPG system highlight broader indications and faster review paths.
| Feature | What to expect | Why it matters |
|---|---|---|
| Power | Rechargeable vs nonrechargeable options | Battery life affects follow‑up and convenience |
| Programming | Paresthesia vs paresthesia‑free modes; clinician ecosystems | Personalized settings improve day‑to‑day relief |
| MRI labeling | Vendor‑specific conditional labeling | Impacts imaging access and long‑term planning |
| Support | Training, customer service, and clinic partnerships | Center experience influences outcomes and adherence |
Competition drives R&D into simpler implants, better programming tools, and noninvasive options for headache and other targets. Insurance coverage in the U.S. varies by plan and indication, so ask clinicians about evidence and expected management steps.
Practical tip: discuss brand features that matter to you—battery type, MRI needs, programming ease, and follow‑up—so you get a device that fits daily life and long‑term pain management.
Programming, follow‑up, and living with a neurostimulation device
Hands-on tuning after surgery turns a functioning device into personalized pain relief.
Initial programming happens within days to weeks after implant. Clinicians set waveforms and location, then refine settings over multiple visits until comfort and coverage improve.
The patient controller lets users switch programs, ramp intensity up or down, and schedule lower settings at night or higher levels for activity. Small changes often restore coverage when symptoms shift.
Practical living tips: follow incision care, adopt safe body mechanics while leads settle, and keep regular charging routines for rechargeable devices. Carry ID for airport screening and check MRI conditional labels before scans.
Track daily pain, sleep, and steps to guide programming adjustments and measure quality life gains. Call your clinic for unusual sensations, sudden loss of coverage, or device alerts; many issues respond to a quick reprogram.
“Expert programming plus engaged self‑management helps patients get the most from neurostimulation day to day.”
| Feature | What to expect | Patient tip |
|---|---|---|
| Follow‑up visits | Iterative adjustments in clinic | Bring a symptom diary to each visit |
| Controller use | Multiple programs and intensity ramps | Practice switching modes at home |
| Battery care | Rechargeable vs non‑rechargeable timelines | Set weekly charge reminders if needed |
| Coordination | Works with PT, meds, and injections | Share device settings with your care team |
Cost, insurance coverage, and access to treatment options
Knowing likely costs, coverage rules, and assistance pathways makes the pathway to care less stressful.
Typical cost components include pre‑implant evaluation and psychological screening, a trial procedure, implant surgery, the device hardware, and follow‑up programming visits. Each step carries clinic, facility, and vendor charges.
U.S. payers evaluate coverage based on evidence and approved indications (FDA, CE Mark, MDR, TGA). Insurance often requires failed conservative therapies and a successful trial before authorizing an implant.
- Work with your clinic’s financial coordinator to verify benefits and secure preauthorization.
- Coverage varies by plan and indication; appeals with specialist documentation can help.
- Manufacturers may provide education, logistical support, and limited financial assistance.
Practical notes: noninvasive devices can sometimes start sooner while implant approvals run. Ask about center experience—efficient programs may lower complication‑related costs. Also consider long‑term value: fewer ER visits, lower medication use, and improved quality life may offset upfront expense.
“Proactive communication with payers and providers keeps timelines clear from evaluation through follow‑up.”
Conclusion
For many patients, electrical stimulation now offers a realistic path to lower pain and improved daily function.
Neurostimulation devices have helped people for more than 40 years. Modern options range from noninvasive tools to implantable systems like SCS, DRG, PNS, VNS, and DBS. When conservative care fails, these devices can be a valuable treatment in a plan for chronic pain.
Careful evaluation, a trial period, and teamwork with rehab and behavioral care boost chances for lasting relief and better quality life. Risks exist but fall with experienced teams, good selection, and close follow-up.
Talk with a pain specialist about which nerve stimulation pathway fits your goals and daily routine. Innovation from Abbott, Medtronic, Boston Scientific, and others keeps expanding options and hope in pain management.

